Controversies in Cardiology. Part 1. Should I treat a high risk chronic coronary syndrome invasively from the beginning? yes, in most cases
DOI:
https://doi.org/10.47487/apcyccv.v1i4.86Keywords:
Coronary disease, angina pectoris, myocardial revascularizationAbstract
Chronic coronary syndrome (SCC) previously known as stable coronary disease, is the main cause of mortality in the world, and it is one of the most important in Peru. This pathology has a dynamic nature that results in different clinical scenarios that can be modified through various therapeutic options, one of which is coronary interventional treatment, mainly in patients with high ischemic risk defined as ischemia greater than 10% of the entire left ventricular mass. For this reason, we have analyzed the most relevant and current information available, concluding that the treatment of high ischemic risk´s chronic coronary syndrome, after an individual evaluation, would correspond to an invasive management from the beginning, although it would not impact on mortality or cardiovascular events, it would contribute to improve quality of life; also we should consider the incomplete availability of all the therapeutic options for the symptomatic management of this disease, the limited access to the management of acute cardiovascular events in our country, as well as the risk of adverse effects and drug interactions.
Downloads
References
Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). Eur Heart J. 2020;41(3):407-77. https://doi.org/10.1093/eurheartj/ehz425.
World Health Organization. Disease burden and mortality estimates [Internet]; [citado 13 de septiembre de 2020]. Disponible en: http://www.who.int/healthinfo/global_burden_disease/estimates/en/
Ministerio de Salud - MINSA [Internet]. [citado 13 de septiembre de 2020]. Disponible en: https://www.gob.pe/minsa.
Hachamovitch R, Hayes SW, Friedman JD, et al. Comparison of the Short-Term Survival Benefit Associated with Revascularization Compared with Medical Therapy in Patients with No Prior Coronary Artery Disease Undergoing Stress Myocardial Perfusion Single Photon Emission Computed Tomography. Circulation. 2003;107(23):2900-7.
https://doi.org/10.1161/01.cir.0000072790.23090.41.
Yoda S, Hori Y, Hayase M, et al. Correlation between early revascularization and major cardiac events demonstrated by ischemic myocardium in Japanese patients with stable coronary artery disease. Journal of Cardiology 71 (2018): 44–51. https://doi.org/10.1016/j.jjcc.2017.05.008.
Patel K, Spertus J, Chan P, et al. Extent of Myocardial Ischemia on Positron Emission Tomography and Survival Benefit with Early Revascularization. J Am Coll Cardiol 2019;74:1645–54. https://doi.org/10.1016/ j.jacc.2019.07.055.
Miller R, Bonow R, Gransar H, et al. Percutaneous or surgical revascularization is associated with survival benefit in stable coronary artery disease. European Heart Journal - Cardiovascular Imaging (2020) 21, 961–70. https://doi.org/10.1093/ehjci/jeaa083.
Azadani P, Miller R, Sharir T, et al. Impact of Early Revascularization on Major Adverse Cardiovascular Events in Relation to Automatically Quantified Ischemia. [Internet]. [citado 19 de agosto de 2020];0(0). Disponible en: https://doi.org/10.1016/j.jcmg.2020.05.039.
Parikh R, Liu G, Plomondon M, et al. Utilization and Outcomes of Measuring Fractional Flow Reserve in Patients with Stable Ischemic Heart Disease. J Am Coll Cardiol 2020;75:409–19. https://doi.org/10.1016/j.jacc.2019.10.060.
Sorbets E, Fox KM, Elbez Y, et al. Long-term outcomes of chronic coronary syndrome worldwide: insights from the international CLARIFY registry. Eur Heart J. 2020;41(3):347-56. https://doi.org/10.1093/eurheartj/ehz660.
Boden WE, O’Rourke RA, Teo KK, et al. Optimal Medical Therapy with or without PCI for Stable Coronary Disease. N Engl J Med.2007;356(15):1503-16. https://www.nejm.org/doi/full/10.1056/nejmoa070829.
Neumann FJ, Sousa-Uva M, Ahlsson A, et al. ESC/EACTS Guidelines on Myocardial Revascularization European Heart Journal 2019(40):87–165. https://doi.org/10.1093/eurheartj/ehy394.
Patel MR, Calhoon JH, Dehmer GJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 Appropriate Use Criteria for CoronaryRevascularization in Patients With Stable Ischemic Heart Disease:A Report of the American College of Cardiology Appropriate UseCriteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Am Coll Cardiol.2017;69(17):2212-41. https://doi.org/10.1016/j.jacc.2017.02.001.
Cesar LA, Ferreira JF, Armaganijan D, et al. Guideline for Stable Coronary Artery Disease. Arq Bras Cardiol. 2014;103(2):01-59. https://doi.org/10.5935/abc.2014s004.
Windecker S, Stortecky S, Stefanini GG, et al. Revascularization versus medical treatment in patients with stable coronary artery disease: network meta-analysis. The BMJ [Internet]. [23 de junio de 2014;citado 13 de septiembre de 2020]. https://doi.org/10.1136/bmj.g3859.
SCOT-HEART investigators. CT coronary angiography in patientswith suspected angina due to coronary heart disease (SCOT-HEART):an open-label, parallel-group, multicentre trial. Lancet 2015;385(9985):2383-91. https://doi.org/10.1016/s0140-6736(15)60291-4.
Xaplanteris P, Fournier S, Pijls NHJ, et al. Five-Year Outcomes with PCI Guided by Fractional Flow Reserve. N Engl J Med.2018;379(3):250-9. https://doi.org/10.1056/nejmoa1803538.
Al-Lamee R, Thompson D, Dehbi HM, et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomized controlled trial. Lancet 2018;391(10115):31-40. https://doi.org/10.1016/s01406736(17)32714-9.
Maron DJ, Hochman JS, Reynolds HR, et al. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N Engl J Med.2020;382(15):1395-407. https://doi.org/10.1056/nejmoa1915922
Spilias N, Zorach B, Denby K, Ellis S. The role of ISCHEMIA in stable ischemic heart disease. Cleve Clin J Med 2020;87(7):401-9. https://doi.org/10.3949/ccjm.87a.20033.
Dahal S, Budoff MJ. Failed ISCHEMIA trial or failed ischemia testing. J Invasive Cardiol 2020;32(4):E83-E85.
Spertus JA, Jones PG, Maron DJ, et al. Health-Status Outcomes with Invasive or Conservative Care in Coronary Disease. N Engl J Med 2020;382:1408-19. https://doi.org/10.1056/nejmoa1916370
Meier D, Mahendiran T, Fournier S. Will ISCHEMIA change our daily practice? Cardiovasc Diagn Ther 2020;10(4):908-11.
Lopes RD, Alexander KP, Stevens SR, et al. Initial Invasive versus Conservative Management of Stable Ischemic Heart Disease Patients with a History of Heart Failure or Left Ventricular Dysfunction: Insights from the ISCHEMIA Trial. Circulation [Internet].[citado 13 de septiembre de 2020]. https://doi.org/10.1161/CIRCULATIONAHA.120.050304.
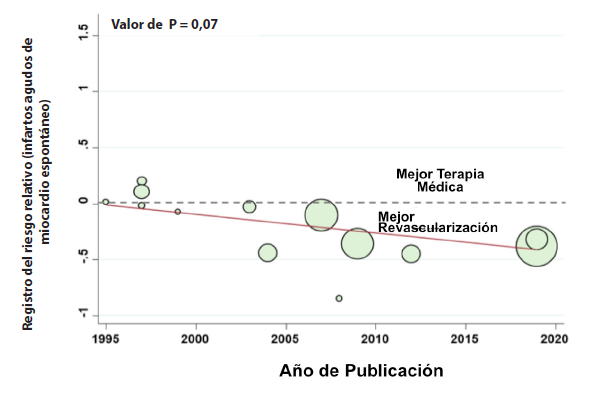
Bangalore S, Maron DJ, Stone GW, et al. Routine Revascularization Versus Initial Medical Therapy for Stable Ischemic Heart Disease. Circulation.2020;142(9):841-57. https://doi.org/10.1161/circulationaha.120.048194.
De Caterina AR, Cuculi F, Banning AP. Incidence, predictors and management of left main coronary artery stent restenosis: a comprehensive review in the era of drug-eluting stents. EuroIntervention 2013;8:1326–34. https://doi.org/10.4244/eijv8i11a201.
Taylor HA, Deumite NJ, Chaitman BR, et al. Asymptomatic left main coronary artery disease in the Coronary Artery Surgery Study (CASS) registry. Circulation 1989; 79:1171–9. https://doi.org/10.1161/01.
CIR.79.6.1171.
Chacón-Diaz M, Vega A, Aráoz O, et al. Características epidemiológicas del infarto de miocardio con elevación del segmento ST en Perú: resultados del PEruvian Registry of ST-segment Elevation Myocardial Infarction (PERSTEMI). Arch Cardiol Mex. 2018;88:403-12. https://doi.org/10.1016/j.acmx.2017.11.009.