Significant valvular heart disease in wild-type transthyretin amyloidosis: prevalence and impact on survival
DOI:
https://doi.org/10.47487/apcyccv.v6i3.524Keywords:
Amyloidosis, Transthyretin, Valvular Heart Diseases, Tricuspid regurgitationAbstract
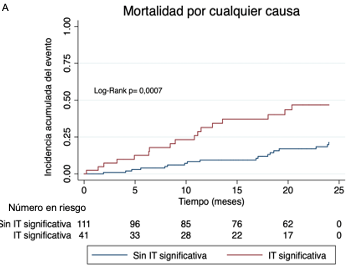
Objective. There are limited data on the prevalence and prognostic impact of significant valvular heart disease in patients with wild-type transthyretin cardiac amyloidosis (ATTRwt). The aim of this study was to describe the prevalence of aortic stenosis (AS), mitral regurgitation (MR), and tricuspid regurgitation (TR) in this population and, secondarily, to evaluate their impact on survival. Methods. This was a retrospective, single-center cohort study including patients diagnosed with ATTRwt between 2011 and 2024. We calculated the prevalence of each significant valvular heart disease, and Kaplan-Meier survival curves were generated to estimate two-year all-cause mortality, stratified according to the presence or absence of each significant valvular disease. Finally, a multivariable Cox regression was performed to assess their association with survival. Results. We included 154 patients, with a mean age of 81 (±7) years; 85% (n=131) were male. Significant TR was the most prevalent valvular disease (27%, n=41), followed by significant MR (20%, n=30) and AS (13%, n=20). Patients with significant TR had a higher incidence of all-cause mortality compared to those without significant TR (41% vs. 16%, log-rank test, p=0.0007), whereas no differences were observed between patients with and without significant AS or MR. In multivariable Cox models, significant TR was independently associated with higher mortality, regardless of age, the presence of other valvular diseases, and NT-proBNP levels. Conclusions. Significant TR was the most prevalent valvular disease in patients with ATTRwt and was associated with lower survival in this population.
Downloads
References
Ruberg FL, Maurer MS. Cardiac Amyloidosis Due to Transthyretin Protein: A Review. JAMA. 2024;331(9):778-91. doi: 10.1001/jama.2024.0442.
González-López E, Gallego-Delgado M, Guzzo-Merello G, de HaroDel Moral FJ, Cobo-Marcos M, Robles C, et al. Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur Heart J. 2015;36(38):2585-94. doi: 10.1093/eurheartj/ehv338.
Decotto S, Fernández Villar G, Llamedo MC, Villanueva E, Pérez De Arenaza D, Lucas L, et al. [Prevalence of transthyretin cardiac amyloidosis in patients hospitalized for heart failure with preserved ejection fraction and septal thickness]. Medicina (B Aires). 2024;84(5):823-30.
García-Pavía P, García-Pinilla JM, Lozano-Bahamonde A, Yun S, GarcíaQuintana A, Gavira-Gómez JJ, et al. Prevalence of transthyretin cardiac amyloidosis in patients with heart failure with preserved ejection fraction: the PRACTICA study. Rev Esp Cardiol (Engl Ed). 2025;78(4):301- 10. doi: 10.1016/j.rec.2024.07.005.
Nativi-Nicolau J, Siu A, Dispenzieri A, Rapezzi C, Kristen AV, GarciaPavia P, et al. Temporal Trends of Wild-Type Transthyretin Amyloid Cardiomyopathy in the Transthyretin Amyloidosis Outcomes Survey. JACC Cardio Oncol. 2021;3(4):537-46. doi: 10.1016/j.jaccao.2021.08.009.
Fontana M, Berk JL, Drachman B, Garcia-Pavia P, Hanna M, Lairez O, et al. Changing Treatment Landscape in Transthyretin Cardiac Amyloidosis. Circ Heart Fail. 2025;e012112. doi: 10.1161/CIRCHEARTFAILURE.124.012112.
Grogan M, Scott CG, Kyle RA, Zeldenrust SR, Gertz MA, Lin G, et al. Natural History of Wild-Type Transthyretin Cardiac Amyloidosis and Risk Stratification Using a Novel Staging System. J Am Coll Cardiol. 2016;68(10):1014-20. doi:10.1016/j.jacc.2016.06.033.
Gillmore JD, Damy T, Fontana M, Hutchinson M, Lachmann HJ, Martinez-Naharro A, et al. A new staging system for cardiac transthyretin amyloidosis. Eur Heart J. 2018;39(30):2799-806. doi: 10.1093/eurheartj/ ehx589.
Ternacle J, Krapf L, Mohty D, Magne J, Nguyen A, Galat A, et al. Aortic Stenosis and Cardiac Amyloidosis: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;74(21):2638-51. doi: 10.1016/j.jacc.2019.09.056.
Castaño A, Narotsky DL, Hamid N, Khalique OK, Morgenstern R, DeLuca A, et al. Unveiling transthyretin cardiac amyloidosis and its predictors among elderly patients with severe aortic stenosis undergoing transcatheter aortic valve replacement. Eur Heart J. 2017;38(38):2879-87. doi: 10.1093/eurheartj/ehx382.
Treibel TA, Fontana M, Gilbertson JA, Castelletti S, White SK, Scully PR, et al. Occult Transthyretin Cardiac Amyloid in Severe Calcific Aortic Stenosis: Prevalence and Prognosis in Patients Undergoing Surgical Aortic Valve Replacement. Circ Cardiovasc Imaging. 2016;9(8):e005066. doi: 10.1161/ CIRCIMAGING.116.005066.
Scully PR, Moon JC, Treibel TA. Cardiac amyloidosis in aortic stenosis: The tip of the iceberg. J Thorac Cardiovasc Surg. 2018;156(3):965-6. doi: 10.1016/j.jacc.2017.11.037.
Dorbala S, Cuddy S, Falk RH. How to Image Cardiac Amyloidosis: A Practical Approach. JACC Cardiovasc Imaging. 2020;13(6):1368-1383. doi: 10.1016/j.jcmg.2019.12.005.
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Fleisher LA, et al. Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25):e1159-e1195. doi: 10.1016/j.jacc.2017.03.011.
Decotto S, Corna G, Villanueva E, Arenaza DP, Seropian I, Falconi M, et al. Prevalence of moderate-severe aortic stenosis in patients with cardiac amyloidosis in a referral center. Arch Cardiol Mex. 2024;94(1):71-8. doi: 10.24875/acm.22000074.
Sperry BW, Jones BM, Vranian MN, Hanna M, Jaber WA. Recognizing Transthyretin Cardiac Amyloidosis in Patients With Aortic Stenosis: Impact on Prognosis. JACC Cardiovasc Imaging. 2016;9(7):904-6. doi: 10.1016/j.jcmg.2015.10.023.
Rosenblum H, Masri A, Narotsky DL, Goldsmith J, Hamid N, Hahn RT, et al. Unveiling outcomes in coexisting severe aortic stenosis and transthyretin cardiac amyloidosis. Eur J Heart Fail. 2021;23(2):250-8. doi:10.1002/ejhf.1974.
Scully PR, Treibel TA, Fontana M, Lloyd G, Mullen M, Pugliese F, et al. Prevalence of Cardiac Amyloidosis in Patients Referred for Transcatheter Aortic Valve Replacement. J Am Coll Cardiol. 2018;71(4):463-4. doi: 10.1016/j.jacc.2017.11.037.
Nitsche C, Scully PR, Patel KP, Kammerlander AA, Koschutnik M, Dona C, et al. Prevalence and Outcomes of Concomitant Aortic Stenosis and Cardiac Amyloidosis. J Am Coll Cardiol. 2021;77(2):128-39. doi:10.1002/ ejhf.2606.
Ho JS-Y, Kor Q, Kong WK, Lim YC, Chan MY, Syn NL, et al. Prevalence and outcomes of concomitant cardiac amyloidosis and aortic stenosis: A systematic review and meta-analysis. Hellenic J Cardiol. 2022;64:67-76. doi: 10.1093/ehjci/jeae060.
Chacko L, Karia N, Venneri L, Bandera F, Passo BD, Buonamici L, et al. Progression of echocardiographic parameters and prognosis in transthyretin cardiac amyloidosis. Eur J Heart Fail. 2022;24(9):1700-12. doi: 10.1002/ejhf.2606.
Tomasoni D, Aimo A, Porcari A, Bonfioli GB, Castiglione V, Saro R, et al. Prevalence and clinical outcomes of isolated or combined moderate to severe mitral and tricuspid regurgitation in patients with cardiac amyloidosis. Eur Heart J Cardiovasc Imaging. 2024;25(7):1007-17. doi: 10.1093/ehjci/jeae060.
Fagot J, Lavie-Badie Y, Blanchard V, Fournier P, Galinier M, Carrié D, et al. Impact of tricuspid regurgitation on survival in patients with cardiac amyloidosis. ESC Heart Fail. 2021;8(1):438-46. doi: 10.1002/ehf2.13093.
Tabata N, Sugiura A, Tsujita K, Nickenig G, Sinning J-M. Percutaneous interventions for mitral and tricuspid heart valve diseases. Cardiovasc Interv Ther. 2020;35(1):62-71. doi: 10.1007/s12928-019-00610-z.
Von Bardeleben RS, Lurz P, Sorajja P, Ruf T, Hausleiter J, Sitges M, et al. Two-Year Outcomes for Tricuspid Repair With a Transcatheter Edge-to-Edge Valve Repair From the Transatlantic TRILUMINATE Trial. Circ Cardiovasc Interv. 2023;16(8):e012888. doi: 10.1161/ CIRCINTERVENTIONS.123.012888.
Schueler R, Hammerstingl C, Werner N, Nickenig G. Interventional Direct Annuloplasty for Functional Tricuspid Regurgitation. JACC Cardiovasc Interv. 2017;10(4):415-416. doi: 10.1016/j.jcin.2016.10.038.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














