Non-valvular infective endocarditis associated with central venous catheter bloodstream infection: a case report
DOI:
https://doi.org/10.47487/apcyccv.v4i4.315Keywords:
Endocarditis, Echocardiography, Three-Dimensional, Central Venous Catheters, Sepsis, Case ReportsAbstract
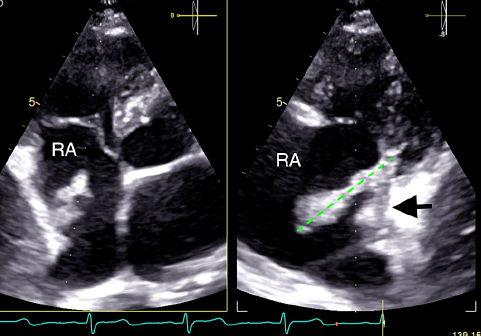
Non-valvular Infective endocarditis (IE) is exceedingly rare; however, its incidence has risen in tandem with the increased usage of intracardiac devices and the growing prevalence of risk factors associated with IE. We present a clinical case involving an 18-year-old patient with IE occurring at an atypical location, concomitant with central venous catheter bloodstream infection. The patient underwent targeted antibiotic therapy but ultimately required surgical resection of the vegetation due to multiple risk factors associated with a poor prognosis. This case underscores the importance of maintaining a low threshold of suspicion for IE and emphasizes the need for heightened vigilance regarding non-valvular tissues hosting foreign bodies. These less common locations pose a risk for vegetation development. Additionally, we underscore the pivotal role of 3D echocardiography tools in anatomically characterizing the vegetation, including dimensions, implantation area, and related anatomy. These tools provide realistic images that facilitate informed decision-making. Furthermore, the timely selection of surgical intervention in patients at elevated risk of therapeutic failure is a cornerstone in effective management.
Downloads
References
Momtazmanesh S, Saeedi Moghaddam S, Malakan Rad E, Azadnajafabad S, Ebrahimi N, Mohammadi E, et al. Global, regional, and national burden and quality of care index of endocarditis: the global burden of disease study 1990–2019. Eur J Prev Cardiol. 2022;29(8):1287-1297. doi: 10.1093/eurjpc/zwab21.
Janszky I, Gemes K, Ahnve S, Asgeirsson H, Moller J. Invasive procedures associated with the development of infective endocarditis. J Am Coll Cardiol. 2018;71(24):2744-2752. doi: 10.1016/j.jacc.2018.03.532.
Pericas JM, Llopis J, Jimenez-Exposito MJ, Kourany WM, Almirante B, Carosi G, et al. Infective endocarditis in patients on chronic hemodialysis. J Am Coll Cardiol. 2021;77(13):1629-1640. doi: 10.1016/j.jacc.2021.02.01.
Kuijpers JM, Koolbergen DR, Groenink M, Peels KCH, Reichert CLA, Post MC, et al. Incidence, risk factors, and predictors of infective endocarditis in adult congenital heart disease: focus on the use of prosthetic material. Eur Heart J. 2017;38(26):2048-2056. doi: 10.1093/eurheartj/ehw591.
Delgado V, Ajmone Marsan N, de Waha S, Bonaros N, Brida M, Burri H, Caselli S, et al. 2023 ESC Guidelines for the management of endocarditis. Eur Heart J. 2023;44(39):3948-4042. doi: 10.1093/eurheartj/ehad193.
Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, et al. 2015 ESC Guidelines for the management of infective endocarditis. Eur Heart J. 2015;36(44):3075-3128. doi: 10.1093/eurheartj/ehv319.
Nassar, GM, Ayus JC. Infectious complications of the hemodialysis access. Kidney Int. 2001;60(1):1-13. doi: 10.1046/j.1523-1755.2001.00765.x.
Thakar S, Janga KC, Tolchinsky T, Greenberg S, Sharma K, Sadiq A, et al. Superior vena cava and right atrium wall infective endocarditis in patients receiving hemodialysis. Heart Lung. 2012;41(3):301-7. doi: 10.1016/j.hrtlng.2011.06.010.
Hoen B, Alla F, Selton-Suty C, Béguinot I, Bouvet A, Briançon S, et al. Changing profile of infective endocarditis: results of a 1-year survey in France. JAMA. 2002;288(1):75-81. doi: 10.1001/jama.288.1.75.
Chrissoheris MP, Libertin C, Ali RG, Ghantous A, Bekui A, Donohue T. Endocarditis complicating central venous catheter bloodstream infections: a unique form of health care associated endocarditis. Clin Cardiol. 2009;32(12):E48-54. doi: 10.1002/clc.20498.
Lorson W, Baljepally G. Cavo-atrial endocarditis: A case of non-valvular endocarditis in a hemodialysis patient. IDCases. 2018;14:e00458. doi: 10.1016/j.idcr.2018.e00458.
Mercado Millan PC, Doval A, Cordero J, Cordova A, Da Silva I, Aguila T, et al. Atrial Masses: a convoluted multimodality diagnosis. J Am Coll Cardiol. 2022;79 (9_Supplement):3034.
Published
Issue
Section
License
Copyright (c) 2023 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














