Quality of life in patients with idiopathic ventricular arrhythmias treated at the Instituto Nacional Cardiovascular - INCOR
DOI:
https://doi.org/10.47487/apcyccv.v4i1.279Keywords:
Arrhythmias, Cardiac, Quality of Life, Anti-Arrhythmia Agents, Catheter AblationAbstract
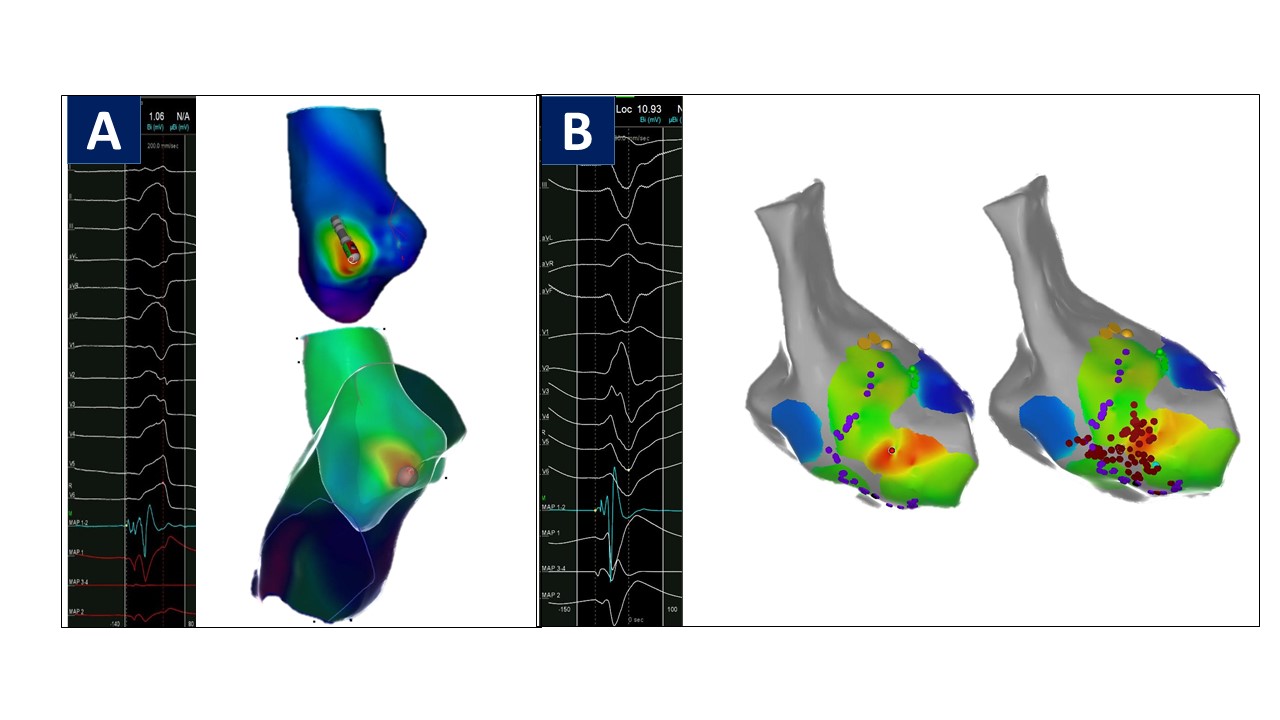
Objective. To describe the quality of life in patients with idiopathic ventricular arrhythmias treated at the Instituto Nacional Cardiovascular INCOR in Lima -Peru. Materials and methods. Analytical and cross-sectional study of patients with idiopathic ventricular arrhythmias treated by 3D ablation or antiarrhythmic therapy between July 2017 and December 2019 to whom the SF-36 health questionnaire was applied to assess quality of life related to health. Results. Fifty-two patients with idiopathic ventricular arrhythmias were included (34 underwent 3D ablation, and 18 underwent antiarrhythmic therapy only). The percentage of recurrence (14.7% vs. 50%, p=0.01) and adverse effects (0% vs. 22.2%, p=0.011) were lower in the 3D ablation group compared to the antiarrhythmic group. The mean standardized scores obtained from the Spanish version of the Health Survey SF-36v2, applied to the 3D ablation and antiarrhythmic groups were 85.1 vs 68.4 (p<0.001), respectively. Were found statistically significant differences in 6 of the eight components that evaluate health-related quality of life: physical function (96.0 vs. 76.0, p<0.001), physical role (93.4 vs. 61.1, p<0.001), general health (74.5 vs. 47.4, p<0.001), vitality (69.9 vs 54.7, p=0.008), emotional role (92.2 vs. 77.8, p=0.006) and mental health (73.8 vs. 60, p<0.001). Conclusions. Patients with idiopathic ventricular arrhythmias who underwent 3D ablation have a higher mean standardized score for health-related quality of life.
Downloads
References
Kobayashi Y. Idiopathic Ventricular Premature Contraction and Ventricular Tachycardia: Distribution of the Origin, Diagnostic Algorithm, and Catheter Ablation. J Nippon Med Sch. 2018;85(2):87- 94. doi: 10.1272/jnms.2018_85-14.
Yamada T. Idiopathic ventricular arrhythmias: Relevance to the anatomy, diagnosis and treatment. J Cardiol. 2016;68(6):463-471. doi: 10.1016/j.jjcc.2016.06.001.
Panizo JG, Barra S, Mellor G, Heck P, Agarwal S. Premature Ventricular Complex-induced Cardiomyopathy. Arrhythm Electrophysiol Rev. 2018;7(2):128-34. doi: 10.15420/aer.2018.23.2.
Tan AY, Ellenbogen K. Ventricular Arrhythmias in Apparently Normal Hearts: Who Needs an Implantable Cardiac Defibrillator? Card Electrophysiol Clin. 2016;8(3):613-21. doi: 10.1016/j.ccep.2016.04.010.
Tondo C, Carbucicchio C, Dello Russo A, Majocchi B, Zucchetti M, Pizzamiglio F, et al. Idiopathic Ventricular Tachycardia: Transcatheter Ablation or AntiarrhythmicDrugs?JAtrFibrillation.2015;7(5):1164.doi:10.4022/jafib.1164.
Duru F. CARTO three-dimensional non-fluoroscopic electroanatomic mapping for catheter ablation of arrhythmias: a useful tool or an expensive toy for the electrophysiologist? Anadolu Kardiyol Derg. 2002;2(4):330-7.
Kim YH, Chen SA, Ernst S, Guzman CE, Han S, Kalarus Z, et al. 2019 APHRS expert consensus statement on three-dimensional mapping systems for tachycardia developed in collaboration with HRS, EHRA, and LAHRS. J Arrhythm. 2020;36(2):215-70. doi: 10.1002/joa3.12308.
Cronin EM, Bogun FM, Maury P, Peichl P, Chen M, Namboodiri N, et al. ESC Scientific Document Group. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Europace. 2019;21(8):1143-1144. doi: 10.1093/ europace/euz132. Erratum in: Europace. 2019;21(8):1144. Erratum in: J Arrhythm. 2020;36(1):214. Erratum in: Europace. 2020;22(3):505.
Huang CX, Liang JJ, Yang B, Jiang H, Tang QZ, Liu XJ, et al. Quality of life and cost for patients with premature ventricular contractions by radiofrequency catheter ablation. Pacing Clin Electrophysiol. 2006;29(4):343-50. doi: 10.1111/j.1540-8159.2006.00351.x.
Urzua M. A, Caqueo-Urizar A. Calidad de vida: Una revisión teórica del concepto. Ter Psicol [online]. 2012;30(1):61-71. doi: 10.4067/ S0718-48082012000100006.
Soto-Becerra R, Taype-Rondan Á, Cabrera-Saldaña M, Guevara- Caicedo C, Zelaya-Castro PD, Medina-Maguiña JM, et al. Ablación de arritmias cardiacas empleando un sistema de mapeo electroanatómico tridimensional en el Instituto Nacional Cardiovascular - INCOR. Arch Peru Cardiol Cir Cardiovasc. 2021;2(3):150-8. doi: 10.47487/apcyccv.v2i3.147.
Alonso J, Prieto L, Anto JM. La versión española del SF-36 Health Survey (Cuestionario de Salud SF-36): un instrumento para la medida de los resultados clínicos. Med Clin (Barc). 1995;104:771-6.
Salazar FR, Bernabé E. The Spanish SF-36 in Peru: factor structure, construct validity, and internal consistency. Asia Pac J Public Health. 2015;27(2):NP2372-80. doi: 10.1177/1010539511432879.
Aksu T, Yalin K, Guler TE, Bozyel S, Heeger CH, Tilz RR. Acute Procedural Complications of Cryoballoon Ablation: A Comprehensive Review. J Atr Fibrillation. 2019;12(3):2208. doi: 10.4022/jafib.2208.
Dan GA, Martinez-Rubio A, Agewall S, Boriani G, Borggrefe M, Gaita F, et al. ESC Scientific Document Group. Antiarrhythmic drugs-clinical use and clinical decision making: a consensus document from the European Heart Rhythm Association (EHRA) and European Society of Cardiology (ESC) Working Group on Cardiovascular Pharmacology, endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS) and International Society of Cardiovascular Pharmacotherapy (ISCP). Europace. 2018;20(5):731-732an. doi: 10.1093/europace/eux373. Erratum in: Europace. 2018;20(5):738.
Zeppenfeld K, Tfelt-Hansen J, de Riva M, Winkel BG, Behr ER, Blom NA, et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022;43(40):3997-4126. doi: 10.1093/eurheartj/ehac262.
Gulletta S, Gasperetti A, Schiavone M, Paglino G, Vergara P, Compagnucci P, et al. Long-Term Follow-Up of Catheter Ablation for Premature Ventricular Complexes in the Modern Era: The Importance of Localization and Substrate. J Clin Med. 2022;11(21):6583. doi: 10.3390/jcm11216583.
Kirchengast S, Haslinger B. Gender differences in health-related quality of life among healthy aged and old-aged Austrians: cross- sectional analysis. Gend Med. 2008;5(3):270-8. doi: 10.1016/j. genm.2008.07.001.
Downloads
Published
Issue
Section
License
Copyright (c) 2023 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














