Clinical variables associated with no-reflow after percutaneous coronary intervention in ST-segment elevation myocardial infarction: Secondary analysis of the PERSTEMI I and II study
DOI:
https://doi.org/10.47487/apcyccv.v3i4.253Keywords:
No-Reflow Phenomenon, ST Elevated Myocardial Infarction, Percutaneous Coronary Intervention, PeruAbstract
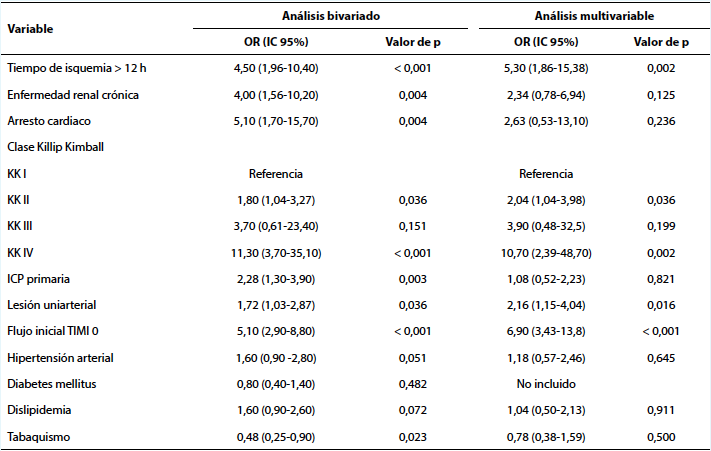
Objective. To determine the clinical factors associated to no-reflow after percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI) in Peru. Materials and methods. Case - control retrospective study, derived from the PERSTEMI (Peruvian Registry of ST-elevation myocardial infarction) I and II study. Cases (group 1) were those patients who presented no-reflow after PCI, defined by a TIMI flow < 3, and controls (group 2) were those with a TIMI 3 flow after the intervention. Clinical and angiographic variables were compared between both groups, and a multivariate analysis was performed looking for associated factors to no-reflow. Results. We included 75 cases and 304 controls. The incidence of no-reflow was 19.8%. There was a higher frequency of no-reflow in patients with primary PCI compared to the pharmacoinvasive strategy, in patients with one-vessel disease and in those with TIMI 0 before PCI. In-hospital mortality and heart failure were higher in patients with no-reflow (21.3% vs. 2.9% and 45.3% vs. 16.5, respectively; p<0.001). After the multivariate analysis, the ischemia time > 12 hours, Killip Kimball (KK) > I, TIMI 0 before PCI, and one-vessel disease were the factors significantly associated with no-reflow after PCI. Conclusions. The ischemia time greater than 12 hours, the highest KK score, the presence of an occluded culprit artery (TIMI 0) before PCI and an one-vessel disease, were factors independently associated to no-reflow in patients with STEMI in Peru.
Downloads
References
Chacón-Diaz M, Rodríguez Olivares R, Miranda-Noé D, Custodio- Sánchez P, Montesinos Cárdenas A, Yábar Galindo G, et al. Tratamiento del infarto agudo de miocardio en el Perú y su relación con eventos adversos intrahospitalarios: resultados del Segundo Registro Peruano de Infarto de Miocardio con elevación del segmento ST (PERSTEMI-II). Arch Peru Cardiol Cir Cardiovasc. 2021;2(2):86-95. doi: 10.47487/apcyccv.v2i2.132.
Chacón-Diaz M, Hernández-Vásquez A, Custodio-Sánchez P. Sobrevida al año en pacientes con infarto de miocardio con elevación del segmento ST en el Perú. Arch Peru Cardiol Cir Cardiovasc. 2022;3(2):53-59. doi: 10.47487/apcyccv.v3i2.218.
Chacón M, Vega A, Aráoz O, Ríos P, Baltodano R, Villanueva F, et al. Características epidemiológicas del infarto de miocardio con elevación del segmento ST en Perú: resultados del PEruvian Registry of ST-segment Elevation Myocardial Infarction (PERSTEMI). Arch Cardiol Mex. 2018;88(5):403-412.
Ibañez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-177. doi: 10.1093/eurheartj/ehx393.
Instituto de Evaluación de Tecnologías en Salud e Investigación. Guía de práctica clínica para el manejo inicial del infarto agudo de miocardio con elevación persistente del segmento ST: Guía en Versión Extensa. Lima: EsSalud; 2022.
Gutiérrez R, Vignolo G, Batista I, Abreu R, Alonso S, Vázquez P, et al. Fenómeno de no reflujo en la angioplastia coronaria: incidencia, características clínico-angiográficas y eficacia del tratamiento. Rev Urug Cardiol 2018;33:279-290. doi: 10.29277/cardio.33.3.7.
Bekkers S, Yazdani S, Virmani R, Waltenberger J, MD. Microvascular obstruction. Underlying pathophysiology and clinical diagnosis. J Am Coll Cardiol. 2010;55(16):1649-60. doi: 10.1016/j.jacc.2009.12.037.
Rezkalla SH, Stankowski RV, Hanna J, Kloner RA. Management of No-Reflow Phenomenon in the Catheterization Laboratory. JACC Cardiovasc Interv. 2017;10(3):215-223. doi: 10.1016/j.jcin.2016.11.059. Erratum in: JACC Cardiovasc Interv. 2017;10(12):1282.
Gagliardi J, Szarferm J, Travetto C, García Escudero A, Gigena G, Rodríguez A, et al. Predictores clínicos de no-reflujo en la angioplastia coronaria por infarto agudo de miocardio. Rev Argent Cardiol. 2013;81:240-245. doi: 10.7775/rac.es.v81.i3.1423.
León Jiménez J, Camacho Freire SJ, Roa Garrido J, Gómez Menchero AE, Cardenal Piris RM, Moraleda Salas MT, et al. Fenómeno de no- reflow coronario: revisión actualizada de un fenómeno antiguo. Cardiocore. 2017;5 2(4):155-161.
Ruíz-Avalos JA, Bazán-Rodríguez L, Espinoza-Escobar G, Martínez- Villa FA, Ornelas-Aguirre JM. Predictors in no-reflow phenomenon in acute myocardial infarction with ST-segment elevation. Arch Cardiol Mex. 2022;92(4):461-468. English. doi: 10.24875/ACM.21000346.
Rivera-Linares BM, Bedolla-Barajas M, Morales-Romero J, Jiménez- Gómez JE. Predictores de fenómeno de no reflujo después de intervención coronaria percutánea primaria. Rev Med Inst Mex Seguro Soc. 2014;52(5):522-9.
Derntl M, Weidinger F. Managing no-reflow during percutaneous coronary intervention. Interv Cardiol. 2012;4(4):461-472.
Kaul S, Methner C, Cao Z, Mishra A. Mechanisms of the “no reflow” phenomenon after acute myocardial infarction. Am J Physiol Heart Circ Physiol. 2021;321(6):H1030-H1041. doi: 10.1152/ ajpheart.00312.2021.
Ndrepepa G, Tiroch K, Fusaro M, Keta D, Seyfarth M, Byrne RA, et al. 5-year prognostic value of no reflow phenomen after percutaneous coronary intervention in patients with acute myocardial infarction. J Am Coll Cardiol. 2010;55(21):2383-9. doi: 10.1016/j.jacc.2009.12.054.
Henriques JP, Zijlstra F, Ottervanger JP, de Boer MJ, van ‘t Hof AW, Hoorntje JC, et al. Incidence and clinical significance of distal embolization during primary angioplasty for acute myocardial infarction. Eur Heart J. 2002;23(14):1112-7. doi: 10.1053/ euhj.2001.3035.
Niccoli G, Kharbanda RK, Crea F, Banning AP. No-reflow: again prevention is better than treatment. Eur Heart J. 2010;31(20):2449- 55. doi: 10.1093/eurheartj/ehq299
Niccoli G, Burzotta F, Galiuto L, Crea F. Myocardial no-reflow in humans. J Am Coll Cardiol. 2009;54(4):281-92. doi: 10.1016/j. jacc.2009.03.054.
Morishima I, Sone T, Okumura K, Tsuboi H, Kondo J, Mukawa H, et al. Angiographic no-reflow phenomenon as a predictor of adverse long- term outcome in patients treated with percutaneous transluminal coronary angioplasty for first acute myocardial infarction. J Am Coll Cardiol. 2000;36(4):1202-9. doi: 10.1016/s0735-1097(00)00865-2.
Muller O, Windecker S, Cuisset T, Fajadet J, Mason M, Zuffi A, et al. Management of two major complications in the cardiac catheterisation laboratory: the no reflow phenomenon and coronary perforations. EuroIntervention. 2008;4(2):181-3. doi: 10.4244/ eijv4i2a32.
Cura FA, García Escudero A, Berrocal D, Mendiz O, Albertal M, Baccaro J, et al. Predictores de reperfusión miocárdica tisular luego de la angioplastia en el infarto agudo de miocardio. Rev Argent Cardiol. 2009;77(3):174-180.
Sorajja P, Gersh BJ, Costantini C, McLaughlin MG, Zimetbaum P, Cox DA, et al. Combined prognostic utility of ST-segment recovery and myocardial blush after primary percutaneous coronary intervention in acute myocardial infarction. Eur Heart J. 2005;26(7):667-74. doi: 10.1093/eurheartj/ehi167.
Ashraf M. Al Azzoni, Lamelas P, Marsden T, Dzavik V, Cairns J, Meeks B, et al. Incidence and predictors of no reflow phenomenon: insights from the total trial. J Am Coll Cardiol. 2017;69(11 Supplement):1179.
Wang JW, Zhou ZQ, Chen YD, Wang CH, Zhu XL. A risk score for no reflow in patients with ST-segment elevation myocardial infarction after primary percutaneous coronary intervention. Clin Cardiol. 2015;38(4):208-15. doi: 10.1002/clc.22376.
Bayramoğlu A, Taşolar H, Kaya A, Tanboğa IH, Yaman M, Bektaş O, et al. Prediction of no reflow and major adverse cardiovascular events with a new scoring system in STEMI patients. J Interv Cardiol. 2018;31(2):144-149. doi: 10.1111/joic.12463.
Deng L, Zhao X, Su X, Zhou M, Huang D, Zeng X. Machine learning to predict no reflow and in-hospital mortality in patients with ST- segment elevation myocardial infarction that underwent primary percutaneous coronary intervention. BMC Med Inform Decis Mak. 2022;22(1):109. doi: 10.1186/s12911-022-01853-2.
Prasad A, Gersh BJ, Mehran R, Brodie BR, Brener SJ, Dizon JM, et al. Effect of Ischemia Duration and Door-to-Balloon Time on Myocardial Perfusion in ST-Segment Elevation Myocardial Infarction: An Analysis From HORIZONS-AMI Trial (Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction). JACC Cardiovasc Interv. 2015;8(15):1966-1974. doi: 10.1016/j. jcin.2015.08.031.
Welsh RC, Van de Werf F, Westerhout CM, Goldstein P, Gershlick AH, Wilcox RG, et al. Outcomes of a pharmacoinvasive strategy for successful versus failed fibrinolysis and primary percutaneous intervention in acute myocardial infarction (from the STrategic Reperfusion Early After Myocardial Infarction [STREAM] study). Am J Cardiol. 2014;114(6):811-9. doi: 10.1016/j.amjcard.2014.06.011.
Nan J, Meng S, Hu H, Jia R, Jin Z. Fibrinolysis therapy combined with deferred PCI versus primary angioplasty for STEMI patients during the COVID-19 pandemic: preliminary results from a single center. Int J Gen Med. 2021;14:201-9. doi: 10.2147/IJGM.S292901.
Chacón-Diaz M, Custodio-Sánchez P, Rojas De la Cuba P, Yábar- Galindo G, Rodríguez-Olivares R, Miranda-Noé D, et al. Outcomes in ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention or pharmacoinvasive strategy in a Latin American country. BMC Cardiovasc Disord. 2022;22(1):296. doi: 10.1186/s12872-022-02730-6.
Braunwald E. Featuring: Eugene Braunwald. Eur Cardiol. 2019;14(2):130-133. doi: 10.15420/ecr.2019.14.2.CM1.
Galiuto L, Lombardo A, Maseri A, Santoro L, Porto I, Cianflone D, et al. Temporal evolution and functional outcome of no reflow: sustained and spontaneously reversible patterns following successful coronary
Paredes-Paucar C, et al. recanalisation. Heart. 2003;89(7):731-7. doi: 10.1136/heart.89.7.731.
Annibali G, Scrocca I, Aranzulla TC, Meliga E, Maiellaro F, Musumeci G. “No-Reflow” Phenomenon: A Contemporary Review. J Clin Med. 2022;11(8):2233. doi: 10.3390/jcm11082233.
O’Farrell FM, Attwell D. A role for pericytes in coronary no-reflow. Nat Rev Cardiol. 2014;11(7):427-32. doi: 10.1038/nrcardio.2014.58.
Li J, Li X, Wang Q, Hu S, Wang Y, Masoudi FA, Spertus JA, Krumholz HM, Jiang L; China PEACE Collaborative Group. ST-segment elevation myocardial infarction in China from 2001 to 2011 (the China PEACE- Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet. 2015;385(9966):441-51. doi: 10.1016/S0140-6736(14)60921-1.
Fineschi M, Verna E, Barioli A, Mezzapelle G, Bartolini D, Turiano G, et al. One-year results from the Assessing MICRO-vascular resistances via IMR to predict outcome in ST-elevation myocardial infarction patients with multivessel disease undergoing primary PCI (AMICRO) trial. Front Cardiovasc Med. 2022;9:1051174. doi: 10.3389/ fcvm.2022.1051174.
Downloads
Published
Issue
Section
License
Copyright (c) 2022 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














