Corrected QT interval and GRACE score relationship in patients with non- ST segment elevation myocardial infarction
DOI:
https://doi.org/10.47487/apcyccv.v3i3.223Keywords:
Corrected QT interval, GRACE score, Non-ST-segment elevation myocardial infarctionAbstract
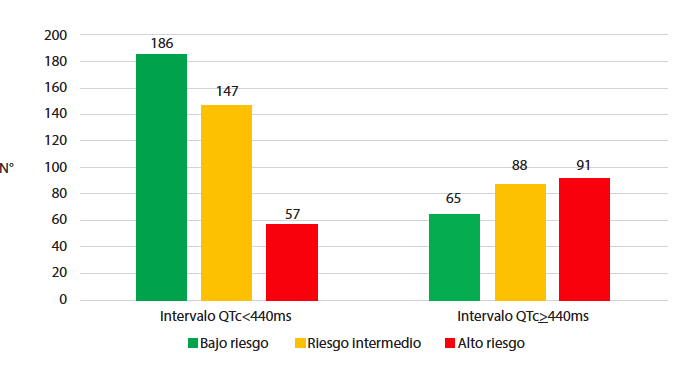
Background. The Global Registry of Acute Coronary Events (GRACE) prediction model stratifies patients with non-ST-segment elevation myocardial infarction (NSTEMI). Corrected QT interval (QTc) is not considered in this model. Objective. To evaluate the relationship between the QTc interval and the GRACE score in patients with NSTEMI. Materials and methods. An observational, retrospective study was carried between 2016 and 2019. We included patients with diagnosis of NSTEMI, QTc intervals were calculated with Bazett’s formula, and they were classified into 2 groups: a normal QTc interval (<440 ms) and prolonged (≥440 ms). According to the GRACE score they were classified in three ranges: low risk (≤109 points), intermedium (110 - 139 points) and high (≥140 points), we determined if there were a correlation between QTc interval and the GRACE score. Results. A total of 940 patients with a diagnosis of NSTEMI were admitted in our institution, 634 met the inclusion criteria, there were 390 patients with normal QTc interval and 244 with a prolonged QTc interval. Patients with prolonged QTc were older (65.5 vs 61, p=0.001) with a lower proportion of males (71.7% vs 82.8%, p=0.001). An association was found between the GRACE score and the QTC interval, subjects with a normal QTc had a greater proportion of low and intermediate risk than those with a prolonged QTc (p=0.001). Conclusions. In NSTEMI patients, a normal QTc interval (<440 ms) is associated with a GRACE risk score of low or intermediate risk.
Downloads
References
Banning AS, Gershlick AH. Timing of intervention in non-ST segment elevation myocardial infarction. Eur Heart J. 2018;20(Suppl B):B10–B20. doi: 10.1093/eurheartj/sux043.
Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42(14):1289-1367. doi: 10.1093/eurheartj/ehaa575.
Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130(25):2354-94. doi: 10.1161/CIR.0000000000000133.
Lee JM, Yoo KD, Oh YS, Kim DB, Park CS, Jang SW, et al. Relationship between resting electrocardiographic parameters and estimated 10-year risk for coronary heart disease in healthy adults in the USA. Ann Noninvasive Electrocardiol. 2010;15(4):315-20. doi: 10.1111/j.1542-474X.2010.00386.x.
Chugh SS, Reinier K, Singh T, Uy-Evanado A, Socoteanu C, Peters D, et al. Determinants of prolonged QT interval and their contribution to sudden death risk in coronary artery disease: the Oregon Sudden Unexpected Death Study. Circulation. 2009;119(5):663-70. doi: 10.1161/CIRCULATIONAHA.108.797035.
Kinoshita T, Asai T, Suzuki T, Matsubayashi K, Horie M. Time course and prognostic implications of QT interval in patients with coronary artery disease undergoing coronary bypass surgery. J Cardiovasc Electrophysiol. 2012;23(6):645-9. doi: 10.1111/j.1540-8167.2011.02244.x.
Zhang Y, Post WS, Blasco-Colmenares E, Dalal D, Tomaselli GF, Guallar E. Electrocardiographic QT interval and mortality: a meta-analysis. Epidemiology. 2011;22(5):660-70. doi: 10.1097/EDE.0b013e318225768b.
Gadaleta FL, Llois SC, Sinisi VA, Quiles J, Avanzas P, Kaski JC. Prolongación del intervalo QT corregido: nuevo predictor de riesgo cardiovascular en el síndrome coronario agudo sin elevación del ST. Rev Esp Cardiol. 2008;61(6):572-8. doi: 10.1157/13123062.
Rajvanshi S, Nath R, Kumar M, Gupta A, Pandit N. Correlation of corrected QT interval with quantitative cardiac troponin-I levels and its prognostic role in Non-ST-elevation myocardial infarction. Int J Cardiol. 2017;240:55-59. doi: 10.1016/j.ijcard.2017.03.091.
Rivera-Fernández R, Arias-Verdú MD, García-Paredes T, Delgado-Rodríguez M, Arboleda-Sánchez JA, Aguilar-Alonso E, et al. Prolonged QT interval in ST-elevation myocardial infarction and mortality: new prognostic scale with QT, Killip and age. J Cardiovasc Med (Hagerstown). 2016;17(1):11-9. doi: 10.2459/JCM.0000000000000015.
Nabati M, Dehghan Z, Kalantari B, Yazdani J. Corrected QT Interval Prolongations in Patients with Non-ST-Elevation Acute Coronary Syndrome. J Tehran Heart Cent. 2018;13(4):173-179.
Bazett HC. An analysis of the time-relations of electrocardiograms. Heart. 1920;7:35-70.
Luo S, Michler K, Johnston P, Macfarlane PW. A comparison of commonly used QT correction formulae: the effect of heart rate on the QTc of normal ECGs. J Electrocardiol. 2004; 37 Suppl: 81-90. doi: 10.1016/j.jelectrocard.2004.08.030.
Bijl M, Verheugt FW. Extreme QT prolongation solely due to reversible myocardial ischemia in single-vessel coronary disease. Am Heart J. 1992;123(2):524-6. doi: 10.1016/0002-8703(92)90672-i.
Kenigsberg DN, Khanal S, Kowalski M, Krishnan SC. Prolongation of the QTc interval is seen uniformly during early transmural ischemia. J Am Coll Cardiol. 2007;49(12):1299-305. doi: 10.1016/j.jacc.2006.11.035
Downloads
Published
Issue
Section
License
Copyright (c) 2022 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














