A randomized controlled trial of ivabradine in patients with acute myocardial infarction related cardiogenic shock
DOI:
https://doi.org/10.47487/apcyccv.v5i2.342Palabras clave:
Ivabradine, Acute Myocardial Infarction, Cardiogenic Shock, Tachycardia, Cardiac Output, Pulmonary Artery CatheterizationResumen
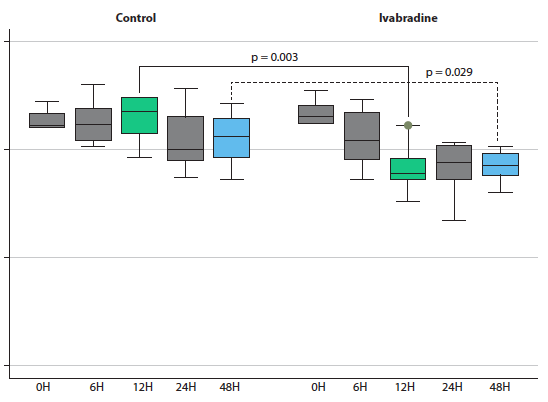
Objective. Acute myocardial infarction-related cardiogenic shock (AMI-CS) is often accompanied by tachycardia, which, in turn, increases myocardial oxygen consumption and hinders the use of ventricular assist devices, such as intra-aortic balloon pump. Evidence suggests that ivabradine may reduce heart rate (HR) without affecting other hemodynamic parameters. The aim of the present study was to determine the effect of ivabradine on reducing HR and changes in other hemodynamic parameters such as cardiac index (CI), in patients with AMI-CS and tachycardia. Materials and methods. A single-center, open label, randomized clinical trial included patients diagnosed with AMI-CS and tachycardia with >100 beats per minute (BPM). Heart rate, cardiac index, and other hemodynamic parameters measured by pulmonary flotation catheter were compared at 0, 6, 12, 24, and 48 hours after randomization. Results. A total of 12 patients were randomized; 6 received standard therapy, and 6 received ivabradine in addition to standard therapy. Baseline clinical characteristics were similar at randomization. A statistically significant lower heart rate was found at 12 hours (p=0.003) and 48 hours (p=0.029) after randomization, with differences of -23.3 (-8.2 to -38.4) BPM and -12.6 (-0.5 to -25.9) BPM, respectively. No differences in cardiac index, or any other evaluated hemodynamic parameters, length of hospital stay, nor mortality rate were noted between both groups. Conclusions. The use of ivabradine in patients with AMI-CS was associated with a significant reduction in heart rate at 12 and 48 h, without affecting other hemodynamic parameters.
Descargas
Referencias
Thiele H, Ohman EM, Desch S, Eitel I, de Waha S. Management of cardiogenic shock. Eur Heart J. 2015;36(20):1223-30. doi: 10.1093/eurheartj/ehv051.
Chioncel O, Parissis J, Mebazaa A, Thiele H, Desch S, Bauersachs J, et al. Epidemiology, pathophysiology and contemporary management of cardiogenic shock – a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2020;22(8):1315-1341. doi: 10.1002/ejhf.1922.
Tehrani BN, Truesdell AG, Psotka MA, Rosner C, Singh R, Sinha SS, et al. A Standardized and Comprehensive Approach to the Management of Cardiogenic Shock. JACC: Heart Fail. 2020;8(11):879-891. doi: 10.1016/j.jchf.2020.09.005.
Padilla-Flores T, López-González Z, Vaca L, Aparicio-Trejo OE, Briones-Herrera A, Riveros-Rosas H, et al. “Funny” channels in cardiac mitochondria modulate membrane potential and oxygen consumption. Biochem Biophys Res Commun. 2020;524(4):1030-6. doi: 10.1016/j.bbrc.2020.02.033.
Koruth JS, Lala A, Pinney S, Reddy VY, Dukkipati SR. The clinical use of ivabradine. J Am Coll Cardiol. 2017;70(14):1777-84. doi: 10.1016/j.jacc.2017.08.038.
Ide T, Ohtani K, Higo T, Tanaka M, Kawasaki Y, Tsutsui H. Ivabradine for the treatment of cardiovascular diseases. Circ J. 2019;83(2):252-60. doi: 10.1253/circj.cj-18-1184.
Koruth JS, Lala A, Pinney S, Reddy VY, Dukkipati SR. The Clinical Use of Ivabradine. J Am Coll Cardiol. 2017;70(14):1777-1784. doi: 10.1016/j.jacc.2017.08.038.
Post F, Münzel T. Ivabradin - eine neue therapieoption bei kardiogenem schock? Herz. 2009;34(3):224-9.
Brunton LL. Goodman & Gilman. Las bases Farmacológicas de la Terapéutica 13a Edición. McGraw Hill Castellano; 2018.
Bonadei I, Sciatti E, Vizzardi E, D’Aloia A, Metra M. Ivabradine during cardiogenic shock: A clinical case and review of the literature. Heart Lung. 2015;44(1):57-8. doi: 10.1016/j.hrtlng.2014.08.003.
Pascual Izco M, Alonso Salinas GL, Sanmartín Fernández M, Del Castillo Carnevalli H, Jiménez Mena M, Camino López A, et al. Clinical Experience with Ivabradine in Acute Heart Failure. Cardiology. 2016;134(3):372-4. doi: 10.1159/000444845.
Elzeneini M, Aranda JM, Al-Ani M, Ahmed MM, Parker AM, Vilaro JR. Hemodynamic effects of ivabradine use in combination with intravenous inotropic therapy in advanced heart failure. Heart Fail Rev. 2021;26(2):355-361. doi: 10.1007/s10741-020-10029-x.
Akodad M, Lim P, Roubille F. Does ivabradine balance dobutamine effects in cardiogenic shock? A promising new strategy. Acta Physiol. 2016;218(2):73-7. doi: 10.1111/apha.12733.
Vahdatpour C, Collins D, Goldberg S. Cardiogenic shock. J Am Heart Assoc. 2019;8(8):e011991. doi: 10.1161/JAHA.119.011991.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Circulation. 2018;138(20):e618-e651. doi: 10.1161/CIR.0000000000000617.
Brugada J, Katritsis DG, Arbelo E, Arribas F, Bax JJ, Blomström-Lundqvist C, et al. 2019 ESC Guidelines for the management of patients with supraventricular tachycardiaThe Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur Heart J. 2020;41(5):655-720. doi: 10.1093/eurheartj/ehz467.
Chiu MH, Howlett JG, Sharma NC. Initiation of ivabradine in cardiogenic shock. ESC Heart Fail. 2019;1;6(5):1088-91. doi: 10.1002/ehf2.12499.
Tse S, Mazzola N. Ivabradine (Corlanor) for heart failure: The first selective and specific I f inhibitor. P T. 2015;40(12):810-4.
Lattuca B, Roubille F. Ivabradine: A promising drug in cardiogenic shock to prevent the undesirable sinus tachycardia induced by dobutamine? Int J Cardiol. 2015;178:308-10. doi: 10.1016/j.ijcard.2014.09.106.
Gallet R, Ternacle J, Damy T, Guendouz S, Bremont C, Seemann A, et al. Hemodynamic effects of Ivabradine in addition to dobutamine in patients with severe systolic dysfunction. Int J Cardiol. 2014;176(2):450-5. doi: 10.1016/j.ijcard.2014.07.093.
Barillà F, Pannarale G, Torromeo C, Paravati V, Acconcia MC, Tanzilli G, et al. Ivabradine in Patients with ST-Elevation Myocardial Infarction Complicated by Cardiogenic Shock: A Preliminary Randomized Prospective Study. Clin Drug Investig. 2016;36(10):849-56. doi: 10.1007/s40261-016-0424-9.
Tien Y-T, Chen W-J, Huang C-H, Wang C-H, Chen W-T, Hung C-S, et al. The CSP (cardiogenic shock prognosis) score: A tool for risk stratification of cardiogenic shock. Front Cardiovasc Med. 2022;9:842056. doi: 10.3389/fcvm.2022.842056.
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2024 La revista es titular de la primera publicación, luego el autor dando crédito a la primera publicación.

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.

















