Recurrent pulmonary thromboembolism with cardiac tamponade as initial manifestations of lupus and antiphospholipid syndrome: a case report
DOI:
https://doi.org/10.47487/apcyccv.v5i4.418Palabras clave:
Lupus Erythematosus, Systemic, Pulmonary Embolism, Antiphospholipid Syndrome, Cardiac TamponadeResumen
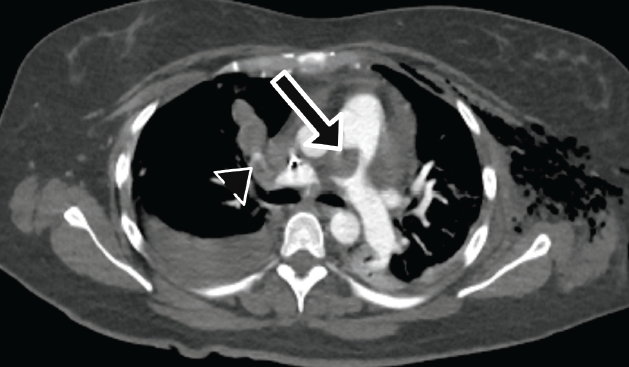
Systemic lupus erythematosus (SLE) is an inflammatory autoimmune disease with an important course due to systemic compromise. SLE is frequently associated with antiphospholipid syndrome, and pulmonary thromboembolism (PE) is particularly common. It is extremely rare for PE to be the initial clinical presentation and even more uncommon for it to coincide with cardiac tamponade, representing a challenge in diagnosis and management. We present a case of a 42-year-old woman with recurrent PE with severe pleural and pericardial effusion, hemodynamic instability, and cardiac tamponade. Laboratory workup revealed hypocomplementemia, leukopenia, negative SLE antibodies, and a positive lupus anticoagulant. This case emphasizes the importance of determining the etiology of PE, assessing risk classification, and implementing proper management, which are crucial for the patient's survival and outcome.
Descargas
Referencias
Benvenuti F, Gatto M, Larosa M, Iaccarino L, Punzi L, Doria A. Cardiovascular risk factors, burden of disease and preventive strategies in patients with systemic lupus erythematosus: a literature review. Expert Opin Drug Saf. 2015;14(9):1373-85. doi: 10.1517/14740338.2015.1073259.
Yafasova A, Fosbøl EL, Schou M, Baslund B, Faurschou M, Docherty KF, et al. Long-Term Cardiovascular Outcomes in Systemic Lupus Erythematosus. J Am Coll Cardiol. 2021;77(14):1717-1727. doi: 10.1016/j.jacc.2021.02.029.
Aviña-Zubieta JA, Vostretsova K, De Vera M, Sayre EC, Choi HK. The Risk of Pulmonary Embolism and Deep Venous Thrombosis in Systemic Lupus Erythematosus: A General Population-Based Study. Semin Arthritis Rheum. 2015;45(2):195-201. doi: 10.1016/j.semarthrit.2015.05.008.
Hisada R, Atsumi T. An Antiphospholipid Antibody Profile as a Biomarker for Thrombophilia in Systemic Lupus Erythematosus. Biomolecules. 2023;13(4):617. doi: 10.3390/biom13040617.
Brouwer JLP, Bijl M, Veeger NJGM, Kluin-Nelemans HC, van der Meer J. The contribution of inherited and acquired thrombophilic defects, alone or combined with antiphospholipid antibodies, to venous and arterial thromboembolism in patients with systemic lupus erythematosus. Blood. 2004;104(1):143-8. doi: 10.1182/blood-2003-11-4085.
Lee JJ, Pope JE. A meta-analysis of the risk of venous thromboembolism in inflammatory rheumatic diseases. Arthritis Res Ther. 2014;16(5):435. doi: 10.1186/s13075-014-0435-y.
Miranda S, Park J, Gal GL, Piran S, Kherani S, Rodger MA, et al. Prevalence of confirmed antiphospholipid syndrome in 18‐50 years unselected patients with first unprovoked venous thromboembolism. J Thromb Haemost. 2020;18(4):926-930. doi: 10.1111/jth.14720.
Tselios K, Urowitz MB. Cardiovascular and Pulmonary Manifestations of Systemic Lupus Erythematosus. Curr Rheumatol Rev. 2017;13(3):206-218. doi: 10.2174/1573397113666170704102444.
Cervera R, Khamashta MA, Font J, Sebastiani GD, Gil A, Lavilla P, et al. Morbidity and Mortality in Systemic Lupus Erythematosus During a 10-Year Period: A Comparison of Early and Late Manifestations in a Cohort of 1,000 Patients. Medicine (Baltimore). 2003;82(5):299-308. doi: 10.1097/01.md.0000091181.93122.55.
Bello N, Meyers KJ, Workman J, Marcano Belisario J, Cervera R. Systematic Literature Review and Meta-analysis of Venous Thromboembolism Events in Systemic Lupus Erythematosus. Rheumatol Ther. 2023;10(1):7-34. doi: 10.1007/s40744-022-00513-1.
Farmer-Boatwright MK, Roubey RAS. Venous Thrombosis in the Antiphospholipid Syndrome. Arterioscler Thromb Vasc Biol. 2009;29(3):321-5. doi: 10.1161/ATVBAHA.108.182204.
Swigris JJ, Fischer A, Gilles J, Meehan RT, Brown KK. Pulmonary and Thrombotic Manifestations of Systemic Lupus Erythematosus. Chest. 2008;133(1):271-80. doi: 10.1378/chest.07-0079.
Aringer M, Costenbader K, Daikh D, Brinks R, Mosca M, Ramsey-Goldman R, et al. 2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus. Arthritis Rheumatol. 2019;71(9):1400-1412. doi: 10.1002/art.40930.
Al-Banaa K, Herrman E, Antonios B, Ahaneku H, Shrotriya S, Wang C, et al. Assessing the Rate of Compliance with the Revised Sapporo/Sydney Criteria in Diagnosing Antiphospholipid Syndrome: A Multicenter Retrospective Analysis. Blood. 2022;140(Supplement 1):2795-6. doi: 10.1182/blood-2022-157217.
Demir S, Li J, Magder LS, Petri M. Antiphospholipid patterns predict risk of thrombosis in systemic lupus erythematosus. Rheumatology (Oxford). 2021;60(8):3770-3777. doi: 10.1093/rheumatology/keaa857.
Garcia D, Erk an D. Diagnosis and Management of the Antiphospholipid Syndrome. N Engl J Med. 2018;378(21):2010-2021. doi: 10.1056/NEJMra1705454.
Schreiber K, Sciascia S, de Groot PG, Devreese K, Jacobsen S, Ruiz-Irastorza G, et al. Antiphospholipid syndrome. Nat Rev Dis Primers. 2018;4:17103. doi: 10.1038/nrdp.2017.103.
Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543-603. doi: 10.1093/eurheartj/ehz405.
Rosenbaum E, Krebs E, Cohen M, Tiliakos A, Derk C. The spectrum of clinical manifestations, outcome and treatment of pericardial tamponade in patients with systemic lupus erythematosus: a retrospective study and literature review. Lupus. 2009;18(7):608-12. doi: 10.1177/0961203308100659.
Harnett DT, Chandra-Sekhar HB, Hamilton SF. Drug-induced lupus erythematosus presenting with cardiac tamponade: a case report and literature review. Can J Cardiol. 2014;30(2):247.e11-2. doi: 10.1016/j.cjca.2013.11.011.
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2024 La revista es titular de la primera publicación, luego el autor dando crédito a la primera publicación.

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.

















