Comparative analysis of myocardial deformation in patients recovered from mild SARS-CoV-2 infection
DOI:
https://doi.org/10.47487/apcyccv.v2i4.175Keywords:
Echocardiography, Ventricular disfunction, left, SARS-CoV-2Abstract
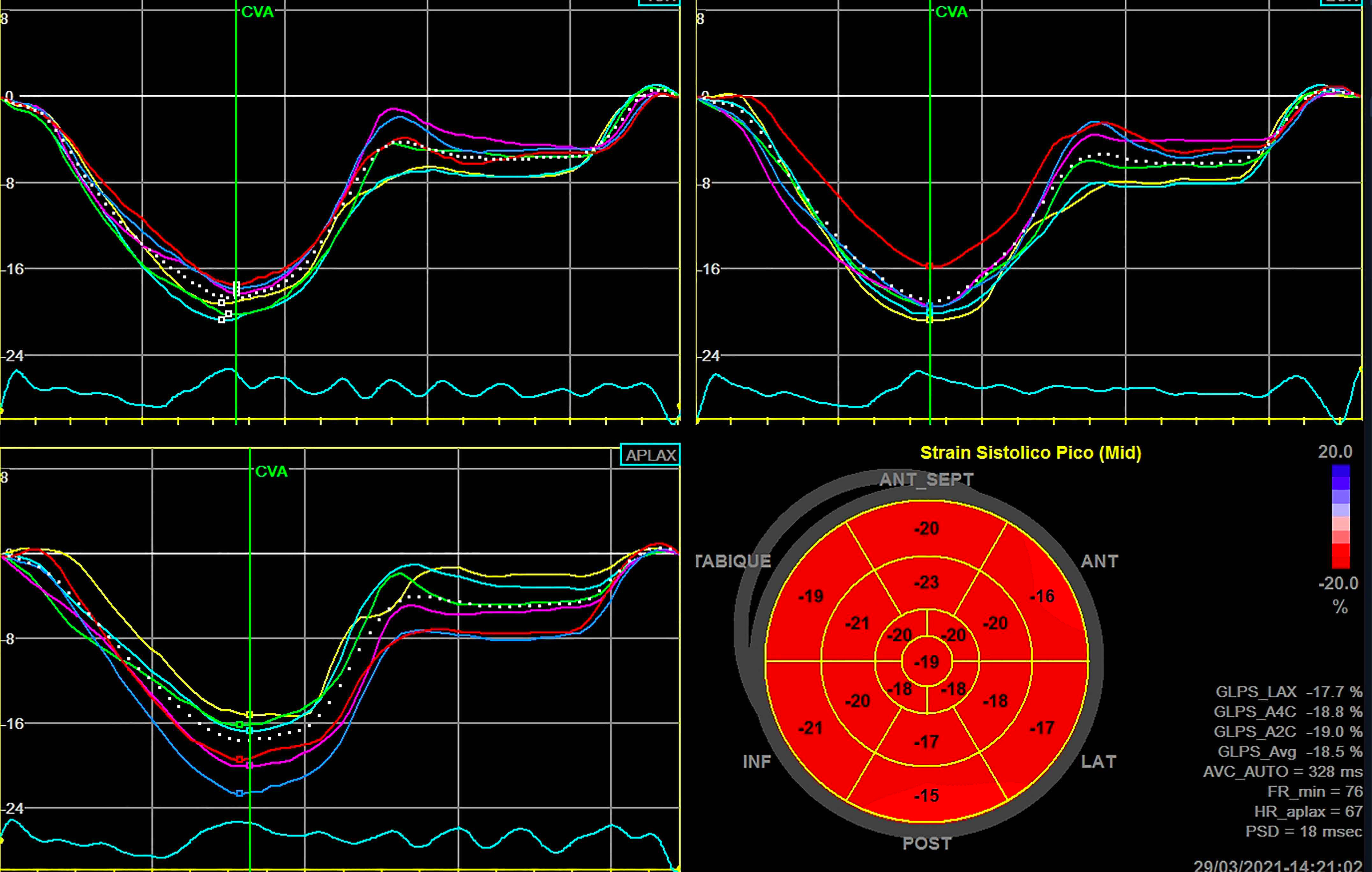
Objectives. During acute infection by the SARS-CoV-2 virus, myocardial involvement has been demonstrated; it is unknown if cardiovascular sequelae in patients recovered from this infection and if these are associated with global morbidity and mortality. The objective of this study was to compare myocardial deformation in patients recovered from mild SARS-CoV-2 virus infection with healthy controls. Materials and methods. This was a cross-sectional observational study that included 33 subjects recovered from mild SARS-CoV-2 infection, who were diagnosed in the previous three to six months, and 31 healthy volunteers, both groups free of cardiovascular risk factors. The study of myocardial deformation was performed using echocardiography with the speckle tracking modality. Clinical and anthropometric variables were compared. Results. The 2D global longitudinal strain of the left ventricle was lower in the subjects recovered from mild SARS-CoV-2 infection than the controls (-20.2% ± 2.6 v -21.6% ± 2.4; p: 0.036). Both groups presented differences in the three ventricular levels, significant at the apical level (-21.2 ± 4.0 vs -23.4% ± 4.2; p: 0.044). The effect by levels shows an inverse Takotsubo pattern. The left ventricular ejection fraction was preserved in both groups (p: 0.153). Conclusions. Left ventricular myocardial deformation is affected in subjects recovered from mild SARS-CoV-2 infection, while the ejection fraction was found in normal ranges. Our study shows a potential role of global longitudinal strain in the detection of subclinical myocardial alterations in patients who had SARS-CoV-2.
Downloads
References
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-733. doi: 10.1056/NEJMoa2001017.
Goerlich E, Gilotra NA, Minhas AS, Bavaro N, Hays AG, Cingolani OH. Prominent Longitudinal Strain Reduction of Basal Left Ventricular Segments in Patients With Coronavirus Disease-19. J Card Fail. 2021;27(1):100-104. doi:10.1016/j.cardfail.2020.09.469.
Puntmann VO, Carerj L, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered from Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265-1273. doi: 10.1001/jamacardio.2020.3557.
Xie Y, Wang L, Li M, Li H, Zhu Sh, Wang B, et al. Biventricular Longitudinal Strain Predict Mortality in COVID-19 Patients. Front Cardiovasc Med. 2021 Jan 18;7:632434. doi: 10.3389/fcvm.2020.632434.
Shmueli H, Shah M, Ebinger JE, Nguyen L-C, Chernomordik F, Flint N, et al. Left ventricular global longitudinal strain in identifying subclinical myocardial dysfunction among patients hospitalized with COVID-19. Int J Cardiol Heart Vasc. 2021;32:100719. doi: 10.1016/j.ijcha.2021.100719.
Wibowo A, Pranata R, Astuti A, Tiksnadi BB, Martanto E, Martha JW, et al. Left and right ventricular longitudinal strains are associated with poor outcome in COVID-19: a systematic review and meta-analysis. J Intensive Care. 2021;9(1):9. doi: 10.1186/s40560-020-00519-3.
Rothschild E, Baruch G, Szekely Y, Lichter Y, Kaplan A, Taieb Ph, et al. The Predictive Role of Left and Right Ventricular Speckle-Tracking Echocardiography in COVID-19. JACC Cardiovasc Imaging. 2020;13(11):2471-2474. doi: 10.1016/j.jcmg.2020.07.026.
Liang T, Cai H, Chen Y, Chen Z, Fang Q, Han W, et al. Handbook of COVID-19 Prevention and Treatment [Internet]. Zhejiang: Universidad de Zhejiang; 2020 [citado el 29 marzo de 2020]. Disponible en: https://gmcc.alibabadoctor.com/preventionmanua
Cupe K, Barrantes C, Meneses G, Rafael E, Lévano G, Baltodano R. Deformación miocárdica bidimensional y tridimensional en una población peruana de adultos sanos. Rev Peru Cardiol. 2019;45(2):79-83.
Sociedad Interamericana de Cardiología. Sobre pandemia COVID-19 y el posible impacto en el funcionamiento de laboratorios de Ecocardiografía [Intenet]. SIAC; 2020 [citado el 29 marzo de 2020]. Disponible: http://www.siacardio.com/consejos/sisiac/editorialessisiac/sisiac-sobre-pandemia-covid-19-y-el-posible-impacto-en-elfuncionamiento-de-laboratorios-de-ecocardiografia/.
Siripanthong B, Nazarian S, Muser D, Deo R, Santangeli P, Khanji MY, et al. Recognizing COVID-19-related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020;17(9):1463-1471. doi: 10.1016/j.hrthm.2020.05.001.
Karamitsos TD, Arvanitaki A., Karvounis H, Neubauer S, Ferreira VM. Myocardial Tissue Characterization and Fibrosis by Imaging. JACC Cardiovasc Imaging. 2020;13(5):1221-1234. doi: 10.1016/j.jcmg.2019.06.030.
Stöbe S, Richter S, Seige M, Stehr S, Laufs U, Hagendorff A. Echocardiographic characteristics of patients with SARS-CoV-2 infection. Clin Res Cardiol. 2020;109(12):1549-1566. doi:10.1007/s00392-020-01727-5.
Kostakou PM, Kostopoulos VS, Tryfou ES, Giannaris VD, Rodis IE, Olympios CD, et al. Subclinical left ventricular dysfunction and correlation with regional strain analysis in myocarditis with normal ejection fraction. A new diagnostic criterion. Int J Cardiol. 2018;259:116-121. doi:10.1016/j.ijcard.2018.01.058.
Kocabay G, Muraru D, Peluso D, Cucchini U, Mihaila S, Padayattil-Jose S, et al. Normal left ventricular mechanics by two-dimensional speckle-tracking echocardiography. Reference values in healthy adults. Rev Esp Cardiol (Engl Ed). 2014;67(8):651-8. doi: 10.1016/j.rec.2013.12.009.