Different phenotypes of mitral regurgitation in patients with right apical ventricular pacing: An echocardiographic approach in a heterogeneity of clinical scenario
DOI:
https://doi.org/10.47487/apcyccv.v2i2.130Keywords:
Mitral regurgitation, Cardiac pacing, Transthoracic echocardiographyAbstract
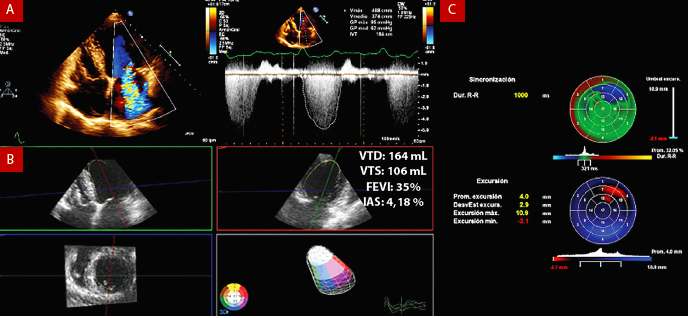
The right ventricular (RV) apical pacing causes a dyssynchronous activation of the left ventricle and the papillary muscles, which determines the decline of the left ventricular ejection fraction (LVEF) in addition to inadequate closure of the valvular apparatus with the presence of different degrees of mitral valve regurgitation. The study of this condition is relevant in clinical decision-making to define patients who benefit from cardiac resynchronization for the relief of symptomatic mitral regurgitation. However, there is a wide heterogeneity of conditions and pathologies that can coexist with different degrees of cardiomyopathies in these patients, which makes etiological determination challenging and worsens the clinical course. The transthoracic echocardiography allows us the comprehensive assessment of mitral valve regurgitation and ventricular function parameters as well as mechanical dyssynchrony as a result of the artificial pacing.
Downloads
References
Gaasch WH, Meyer TE. Secondary mitral regurgitation (part 1): volumetric quantification and analysis. Heart. 2018;104(8):634-638. doi:10.1136/heartjnl-2017-312001
Bonow RO, O’Gara PT, Adams DH, et al. 2020 Focused Update of the 2017 ACC Expert Consensus Decision Pathway on the Management of Mitral Regurgitation: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2020;75(17):2236-2270. doi:10.1016/j.jacc.2020.02.005
Gaasch WH, Meyer TE. Secondary mitral regurgitation (part 2): deliberations on mitral surgery and transcatheter repair. Heart. 2018;104(8):639-643. doi:10.1136/heartjnl-2017-312002
Prinzen FW, Hunter WC, Wyman BT, McVeigh ER. Mapping of regional myocardial strain and work during ventricular pacing: experimental study using magnetic resonance imaging tagging. J Am Coll Cardiol. 1999;33(6):1735-1742. doi:10.1016/s0735-1097(99)00068-6
Tops LF, Suffoletto MS, Bleeker GB, et al. Speckle-Tracking Radial Strain Reveals Left Ventricular Dyssynchrony in Patients With Permanent Right Ventricular Pacing. J Am Coll Cardiol. 2007;50(12):1180-1188. doi:https://doi.org/10.1016/j.jacc.2007.06.011
Ebert M, Jander N, Minners J, et al. Long-Term Impact of Right Ventricular Pacing on Left Ventricular Systolic Function in Pacemaker Recipients with Preserved Ejection Fraction: Results from a Large Single-Center Registry. J Am Heart Assoc. 2016;5(7):e003485. doi:10.1161/JAHA.116.003485
Bartko PE, Arfsten H, Heitzinger G, et al. Papillary Muscle Dyssynchrony-Mediated Functional Mitral Regurgitation: Mechanistic Insights and Modulation by Cardiac Resynchronization. JACC Cardiovasc Imaging. 2019;12(9):1728-1737. doi:10.1016/j.jcmg.2018.06.013
Stone GW, Lindenfeld J, Abraham WT, et al. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N Engl J Med. 2018;379(24):2307-2318. doi:10.1056/NEJMoa1806640
Reddy YN V, Nishimura RA. Not All Secondary Mitral Regurgitation Is the Same-Potential Phenotypes and Implications for Mitral Repair. JAMA Cardiol. July 2020. doi:10.1001/jamacardio.2020.2236
Goldstein D, Moskowitz AJ, Gelijns AC, et al. Two-Year Outcomes of Surgical Treatment of Severe Ischemic Mitral Regurgitation. N Engl J Med. 2016;374(4):344-353. doi:10.1056/NEJMoa1512913
Aguero J, Galan-Arriola C, Fernandez-Jimenez R, et al. Atrial Infarction and Ischemic Mitral Regurgitation Contribute to Post-MI Remodeling of the Left Atrium. J Am Coll Cardiol. 2017;70(23):2878-2889. doi:10.1016/j.jacc.2017.10.013
Nishino S, Watanabe N, Ashikaga K, et al. Reverse Remodeling of the Mitral Valve Complex After Radiofrequency Catheter Ablation for Atrial Fibrillation: A Serial 3-Dimensional Echocardiographic Study. Circ Cardiovasc Imaging. 2019;12(10):e009317. doi:10.1161/CIRCIMAGING.119.009317
Tayal B, Fruelund P, Sogaard P, et al. Incidence of heart failure after pacemaker implantation: a nationwide Danish Registry-based follow-up study. Eur Heart J. 2019;40(44):3641-3648. doi:10.1093/eurheartj/ehz584
Gorcsan J 3rd, Lumens J. Rocking and Flashing with RV Pacing: Implications for Resynchronization Therapy. JACC Cardiovasc Imaging. 2017;10(10 Pt A):1100-1102. doi:10.1016/j.jcmg.2016.09.020
Yu C-M, Zhang Q, Fung JW-H, et al. A novel tool to assess systolic asynchrony and identify responders of cardiac resynchronization therapy by tissue synchronization imaging. J Am Coll Cardiol. 2005;45(5):677-684. doi:10.1016/j.jacc.2004.12.003
Van Everdingen WM, Schipper JC, van ’t Sant J, Ramdat Misier K, Meine M, Cramer MJ. Echocardiography and cardiac resynchronisation therapy, friends or foes? Netherlands Hear J. 2016;24(1):25-38. doi:10.1007/s12471-015-0769-3
Kapetanakis S, Kearney MT, Siva A, Gall N, Cooklin M, Monaghan MJ. Real-time three-dimensional echocardiography: a novel technique to quantify global left ventricular mechanical dyssynchrony. Circulation. 2005;112(7):992-1000. doi:10.1161/CIRCULATIONAHA.104.474445
Delgado V, Sitges M, Vidal B, et al. Assessment of Left Ventricular Dyssynchrony by Real-Time Three-Dimensional Echocardiography. Rev Española Cardiol. 2008;61(8):825-834. doi:10.1016/S1885-5857(08)60230-3
Ivan S, Christian P, Agnieszka C, et al. Long-Term Outcome After CRT in the Presence of Mechanical Dyssynchrony Seen With Chronic RV Pacing or Intrinsic LBBB. JACC Cardiovasc Imaging. 2017;10(10_Part_A):1091-1099. doi:10.1016/j.jcmg.2016.08.015
Lumens J, Tayal B, Walmsley J, et al. Differentiating Electromechanical From Non-Electrical Substrates of Mechanical Discoordination to Identify Responders to Cardiac Resynchronization Therapy. Circ Cardiovasc Imaging. 2015;8(9):e003744. doi:10.1161/CIRCIMAGING.115.003744
Kvitting J-PE, Ebbers T, Engvall J, Sutherland GR, Wranne B, Wigström L. Three-directional myocardial motion assessed using 3D phase contrast MRI. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson. 2004;6(3):627-636. doi:10.1081/jcmr-120038692
Liu W-H, Chen M-C, Chen Y-L, et al. Right ventricular apical pacing acutely impairs left ventricular function and induces mechanical dyssynchrony in patients with sick sinus syndrome: a real-time three-dimensional echocardiographic study. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2008;21(3):224-229. doi:10.1016/j.echo.2007.08.045
Fang F, Chan JY-S, Yip GW-K, et al. Prevalence and determinants of left ventricular systolic dyssynchrony in patients with normal ejection fraction received right ventricular apical pacing: a real-time three-dimensional echocardiographic study. Eur J Echocardiogr. 2010;11(2):109-118. doi:10.1093/ejechocard/jep171
Mehrotra R. Three-dimensional echocardiographic systolic dyssynchrony index- what is the correct cut-off? Indian Heart J. 2018;70(5):765. doi:10.1016/j.ihj.2018.08.020
Packer M, Grayburn PA. Neurohormonal and Transcatheter Repair Strategies for Proportionate and Disproportionate Functional Mitral Regurgitation in Heart Failure. JACC Heart Fail. 2019;7(6):518-521. doi:10.1016/j.jchf.2019.03.016
Packer M, Grayburn PA. Contrasting Effects of Pharmacological, Procedural, and Surgical Interventions on Proportionate and Disproportionate Functional Mitral Regurgitation in Chronic Heart Failure. Circulation. 2019;140(9):779-789. doi:10.1161/CIRCULATIONAHA.119.039612
Packer M, Grayburn PA. New Evidence Supporting a Novel Conceptual Framework for Distinguishing Proportionate and Disproportionate Functional Mitral Regurgitation. JAMA Cardiol. 2020;5(4):469-475. doi:10.1001/jamacardio.2019.5971
Epstein AE, DiMarco JP, Ellenbogen KA, et al. 2012 ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2013;61(3):e6-75. doi:10.1016/j.jacc.2012.11.007
Brignole M, Auricchio A, Baron-Esquivias G, et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J. 2013;34(29):2281-2329. doi:10.1093/eurheartj/eht150
Ypenburg C, Lancellotti P, Tops LF, et al. Mechanism of improvement in mitral regurgitation after cardiac resynchronization therapy. Eur Heart J. 2008;29(6):757-765. doi:10.1093/eurheartj/ehn063
Kanzaki H, Bazaz R, Schwartzman D, Dohi K, Sade LE, Gorcsan J 3rd. A mechanism for immediate reduction in mitral regurgitation after cardiac resynchronization therapy: insights from mechanical activation strain mapping. J Am Coll Cardiol. 2004;44(8):1619-1625. doi:10.1016/j.jacc.2004.07.036
Agricola E, Galderisi M, Mele D, et al. Mechanical dyssynchrony and functional mitral regurgitation: pathophysiology and clinical implications. J Cardiovasc Med (Hagerstown). 2008;9(5):461-469. doi:10.2459/JCM.0b013e3282ef39c5
Matsumoto K, Tanaka H, Okajima K, et al. Relation between left ventricular morphology and reduction in functional mitral regurgitation by cardiac resynchronization therapy in patients with idiopathic dilated cardiomyopathy. Am J Cardiol. 2011;108(9):1327-1334. doi:10.1016/j.amjcard.2011.06.052
Ypenburg C, Lancellotti P, Tops LF, et al. Acute effects of initiation and withdrawal of cardiac resynchronization therapy on papillary muscle dyssynchrony and mitral regurgitation. J Am Coll Cardiol. 2007;50(21):2071-2077. doi:10.1016/j.jacc.2007.08.019
Mihos CG, Yucel E, Capoulade R, et al. Effects of cardiac resynchronization therapy after inferior myocardial infarction on secondary mitral regurgitation and mitral valve geometry. Pacing Clin Electrophysiol. 2018;41(2):114-121. doi:10.1111/pace.13255
Downloads
Additional Files
Published
Issue
Section
License
Copyright (c) 2021 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














