Cardiac magnetic resonance as a risk re-stratification tool in apical hypertrophic cardiomyopathy
DOI:
https://doi.org/10.47487/apcyccv.v4i2.289Palabras clave:
Apical Hypertrophic Cardiomyopathy, Cardiac Aneurysm, Echocardiography, Cardiac Magnetic ResonanceResumen
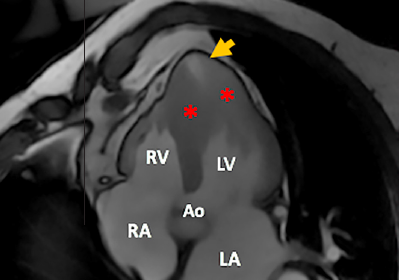
Apical hypertrophic cardiomyopathy (ApHCM) can result in the formation of a left ventricular apical aneurysm and progressive myocardial fibrosis, which is associated with a worse prognosis. We present the case of a 76-year-old man previously diagnosed with ApHCM seven years ago, who has been under clinical follow-up. Serial cardiac magnetic resonance (CMR) imaging was performed in 2013 and 2020 due to suspected apical aneurysm formation based on echocardiographic evaluation. The 2020 CMR imaging revealed an increase in myocardial fibrosis observed through late-gadolinium enhancement images and, for the first time, a small apical aneurysm that was not clearly visualized on two-dimensional echocardiography. The time course leading to the development of an ApHCM aneurysm is not well-defined and may impact the clinical course.
Descargas
Referencias
Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014 Oct;35(39):2733-79. doi: 10.1093/eurheartj/ehu284.
Hughes RK, Knott KD, Malcolmson J, Augusto JB, Mohiddin SA, Kellman P, et al. Apical Hypertrophic Cardiomyopathy: The Variant Less Known. J Am Heart Assoc. 2020 Mar 3;9(5):e015294. doi: 10.1161/JAHA.119.015294.
Chen C-C, Lei M-H, Hsu Y-C, Chung S-L, Sung Y-J. Apical hypertrophic cardiomyopathy: correlations between echocardiographic parameters, angiographic left ventricular morphology, and clinical outcomes. Clin Cardiol. 2011 Apr;34(4):233-8. doi: 10.1002/clc.20874.
Maron MS, Finley JJ, Bos JM, Hauser TH, Manning WJ, Haas TS, et al. Prevalence, clinical significance, and natural history of left ventricular apical aneurysms in hypertrophic cardiomyopathy. Circulation. 2008 Oct;118(15):1541-9. doi: 10.1161/CIRCULATIONAHA.108.781401.
Klarich KW, Attenhofer Jost CH, Binder J, Connolly HM, Scott CG, Freeman WK, et al. Risk of death in long-term follow-up of patients with apical hypertrophic cardiomyopathy. Am J Cardiol. 2013 Jun;111(12):1784-91. doi: 10.1016/j.amjcard.2013.02.040.
Eriksson MJ, Sonnenberg B, Woo A, Rakowski P, Parker TG, Wigle ED, et al. Long-term outcome in patients with apical hypertrophic cardiomyopathy. J Am Coll Cardiol. 2002 Feb;39(4):638-45. doi: 10.1016/s0735-1097(01)01778-8.
patients with ApHCM, aneurysm formation was related to four stages for its development, starting with systolic apical cavity obliteration, then broadening of the apical slit in systole, further developing into an apical outpouching, and finally forming an apical aneurysm. Nevertheless, further investigations are required to clarify time progression and established specific CMR follow- up recommendations.
In conclusion, apical aneurysm detection in ApHCM is a valuable strategy for identifying patients at higher risk of cardiovascular events. Echocardiography is the primary modality for assessment and monitoring, while CMR imaging plays a confirmatory role in inconclusive cases. Regular imaging follow- up is recommended to detect aneurysm formation and assess the progression of myocardial fibrosis, enabling re-evaluation of the risk of SCD. In this case, CMR imaging played a crucial role in re- stratification.
Author ́s contributions: AML and DC: Data curation, investigation, writing, review and editing. SRU, ZV and BF: Writing, review and editing.
Jan MF, Todaro MC, Oreto L, Tajik AJ. Apical hypertrophic cardiomyopathy: Present status. Int J Cardiol. 2016 Nov;222:745- 59. doi: 10.1016/j.ijcard.2016.07.154.
Wigle ED, Rakowski H. Hypertrophic cardiomyopathy: when do you diagnose midventricular obstruction versus apical cavity obliteration with a small nonobliterated area at the apex of the left ventricle? J Am Coll Cardiol. 1992 Mar 1;19(3):525-6. doi: 10.1016/s0735-1097(10)80265-7.
Wilson P, Marks A, Rastegar H, Manolis AS, Estes NA 3rd. Apical hypertrophic cardiomyopathy presenting with sustained monomorphic ventricular tachycardiaandelectrocardiographicchangessimulating coronary artery disease and left ventricular aneurysm. Clin Cardiol. 1990 Dec;13(12):885-7. doi: 10.1002/clc.4960131213.
Ommen SR, Mital S, Burke MA, Day SM, Deswal A, Elliott P, et al. 2020 AHA/ACC Guideline for the Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2020 Dec;142(25):e558-631. doi: 10.1161/ CIR.0000000000000937.
RowinEJ,MaronBJ,HaasTS,GarberichRF,WangW,LinkMS, et al. Hypertrophic Cardiomyopathy With Left Ventricular Apical Aneurysm: Implications for Risk Stratification and Management. J Am Coll Cardiol. 2017 Feb;69(7):761-73. doi: 10.1016/j. jacc.2016.11.063.
Alfonso F, Frenneaux MP, McKenna WJ. Clinical sustained uniform ventricular tachycardia in hypertrophic cardiomyopathy: association with left ventricular apical aneurysm. Br Heart J. 1989 Feb;61(2):178-81. doi: 10.1136/hrt.61.2.178.
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2023 La revista es titular de la primera publicación, luego el autor dando crédito a la primera publicación.

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.

















