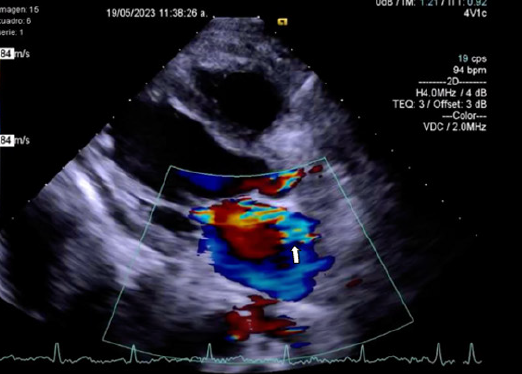
Mitral valve infective endocarditis as a manifestation of disseminated Cryptococcus neoformans infection: a case report
DOI:
https://doi.org/10.47487/apcyccv.v5i4.412Palabras clave:
Cryptococcus neoformans, Endocarditis, Mycoses, Mitral ValveResumen
Infective endocarditis is a disease that affects mainly the endocardial surface of the heart and cardiac valves (native or prosthetic). The main risk factors for developing infective endocarditis are male sex, older age, intracardiac shunts, prosthetic valves, rheumatic, and congenital heart disease, intracardiac devices, intravenous drugs use, immunosuppression, and hemodialysis. Streptococci and Staphylococci spp. have been the most frequent isolated organisms. On the other hand, the most common fungal organism in infective endocarditis is Candida albicans (24-46%), followed by Aspergillus spp. (25%), and a few cases by Cryptococcus neoformans, which are associated with higher rate of mortality. This case provides an interesting case of Cryptococcus neoformans native valve infective endocarditis in a young woman with stage IV chronic kidney disease and severe malnutrition.
Descargas
Referencias
Alspaugh JA. Virulence mechanisms and Cryptococcus neoformans pathogenesis. Fungal Genet Biol. 2015;78:55-8. doi: 10.1016/j.fgb.2014.09.004.
McGuire CN, Walter DJ. Cryptococcus neoformans endocarditis in an immunocompetent patient a case report. BMC Cardiovasc Disord. 2022;22(1):565. doi: 10.1186/s12872-022-02997-9.
Zhao Y, Lin X. Cryptococcus neoformans: Sex, morphogenesis, and virulence. Infect Genet Evol. 2021;89:104731. doi: 10.1016/j.meegid.2021.104731.
Hubers SA, DeSimone DC, Gersh BJ, Anavekar NS. Infective Endocarditis: A Contemporary Review. Mayo Clin Proc. 2020;95(5):982-997. doi: 10.1016/j.mayocp.2019.12.008.
Cimmino G, Bottino R, Formisano T, Orlandi M, Molinari D, Sperlongano S, et al. Current Views on Infective Endocarditis: Changing Epidemiology, Improving Diagnostic Tools and Centering the Patient for Up-to-Date Management. Life. (Basel). 2023;13(2):377. doi: 10.3390/life13020377.
Holland TL, Baddour LM, Bayer AS, Hoen B, Miro JM, Fowler VG Jr. Infective endocarditis. Nat Rev Dis Primers. 2016;2:16059. doi:
1038/nrdp.2016.59. 7. Ruiz-Beltran AM, Barron-Magdaleno C, Ruiz-Beltran SM, Sánchez-Villa JD, Orihuela-Sandoval C, Oseguera-Moguel J, et al. Infective endocarditis: 10-year experience in a non-cardiovascular center. Arch Cardiol Mex. 2022;92(1):5-10. doi: 10.24875/ACM.20000467.
Badiee P, Amirghofran AA, Ghazi Nour M, Shafa M, Nemati MH. Incidence and outcome of documented fungal endocarditis. Int Cardiovasc Res J. 2014;8(4):152-5.
Levitz SM. The ecology of Cryptococcus neoformans and the epidemiology of cryptococcosis. Rev Infect Dis. 1991;13(6):1163-9. doi: 10.1093/clinids/13.6.1163.
Pappas PG. Cryptococcal infections in non-HIV-infected patients. Trans Am Clin Climatol Assoc. 2013;124:61-79.
Espi M, Koppe L, Fouque D, Thaunat O. Chronic Kidney Disease-Associated Immune Dysfunctions: Impact of Protein-Bound Uremic Retention Solutes on Immune Cells. Toxins (Basel). 2020;12(5):300. doi: 10.3390/toxins12050300.
J. Yang, W. He (eds.). Chronic Kidney Disease. Singapore: Springer Nature; 2020. doi: 10.1007/978-981-32-9131-7_12.
Fowler VG, Durack DT, Selton-Suty C, Athan E, Bayer AS, Chamis AL, et al. The 2023 Duke-International Society for Cardiovascular Infectious Diseases Criteria for Infective Endocarditis: Updating the Modified Duke Criteria. Clin Infect Dis. 2023;77(4):518-26. doi: 10.1093/cid/ciad271.
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2024 La revista es titular de la primera publicación, luego el autor dando crédito a la primera publicación.

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.

















