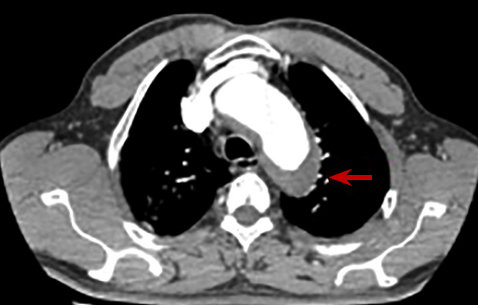
Complex management of intramural hematoma of the descending aorta: about a case
DOI:
https://doi.org/10.47487/apcyccv.v1i3.75Keywords:
chest pain, aortic disease, hematoma, endovascular proceduresAbstract
Acute aortic syndromes (AAS) include a variety of overlapping anatomical and clinical conditions. Intramural hematoma (IMH), penetrating aortic ulcer (UAP), and aortic dissection occur in isolation or may coexist in the same patient. All entities are potentially life threatening, so prompt diagnosis and management are a primary goal of care. IMH represents 5-30% of all AAS and 60-70% of cases are located in the descending portion of the aorta. The diagnosis relies on a high index of clinical suspicion and on the use of complementary images (computed tomography and magnetic resonance imaging). Management is conservative, but patients with persistent pain despite treatment, with hemodynamic instability, with a maximum diameter of the aorta of> 55 mm, with periaortic hemorrhage and focal intimal disruptions have a higher risk of mortality in the acute phase, therefore surgical management should be considered initially endovascular. We present the case of a 69-year-old patient, in whom IMH was diagnosed in the course of a hypertensive emergency and who required hybrid management due to high-risk anatomical characteristics with only endovascular management.
Downloads
References
Evangelista A, Maldonado G, Moral S et al. Intramural hematoma and penetrating ulcer in the descending aorta: differences and similarities. Ann Cardiothorac Surg. 2019 Jul;8(4):456–70.
Nienaber CA, Eagle KA. Aortic dissection: new frontiers in diagnosis and management: Part I: from etiology to diagnostic strategies. Circulation. 2003 Aug 5;108(5):628–35.
Stanson AW, Kazmier FJ, Hollier LH et al. Penetrating atherosclerotic ulcers of the thoracic aorta: natural history and clinicopathologic correlations. Ann Vasc Surg. 1986 May;1(1):15–23.
Maraj R, Rerkpattanapipat P, Jacobs LE et al. Meta-analysis of 143 reported cases of aortic intramural hematoma. Am J Cardiol. 2000 Sep 15;86(6):664–8.
Nauta F, de Beaufort H, Mussa FF, et al. Management of retrograde type A IMH with acute arch tear/type B dissection. Ann Cardiothorac Surg. 2019 Sep;8(5):531–9.
Maslow A, Atalay MK, Sodha N. Intramural Hematoma. J Cardiothorac Vasc Anesth. 2018;32(3):1341–62.
Moral S, Cuéllar H, Avegliano G, et al. Clinical Implications of Focal Intimal Disruption in Patients With Type B Intramural Hematoma. J Am Coll Cardiol. 2017 Jan 3;69(1):28–39.
Choi Y-J, Son J-W, Lee S-H, et al. Treatment patterns and their outcomes of acute aortic intramural hematoma in real world: multicenter registry for aortic intramural hematoma. BMC Cardiovasc Disord. 2014 Aug 19;14:103.
Tolenaar JL, Harris KM, Upchurch GR, et al. The differences and similarities between intramural hematoma of the descending aorta and acute type B dissection. J Vasc Surg. 2013 Dec;58(6):1498–504.
Evangelista A, Mukherjee D, Mehta RH et al. Acute intramural hematoma of the aorta: a mystery in evolution. Circulation. 2005 Mar 1;111(8):1063–70.
Shapira OM, Aldea GS, Cutter SM et al. Improved clinical outcomes after operation of the proximal aorta: a 10-year experience. Ann Thorac Surg. 1999 Apr;67(4):1030–7.
Walsh SR, Tang TY, Sadat U, et al. Endovascular stenting versus open surgery for thoracic aortic disease: systematic review and meta-analysis of perioperative results. J Vasc Surg. 2008 May;47(5):1094–8.
Feezor RJ, Lee WA. Management of the left subclavian artery during TEVAR. Semin Vasc Surg. 2009 Sep;22(3):159–64.
Hajibandeh S, Hajibandeh S, Antoniou SA et al. Meta-analysis of Left Subclavian Artery Coverage With and Without Revascularization in Thoracic Endovascular Aortic Repair. J Endovasc Ther Off J Int Soc Endovasc Spec. 2016 Aug;23(4):634–41.
Conway AM, Qato K, Nguyen Tran N N et al. Management of the Left Subclavian Artery in TEVAR for Chronic Type B Aortic Dissection. Vasc Endovascular Surg. 2020 Jul 23;1538574420942353.