Right ventricular uncoupling in acute heart failure with preserved or mildly reduced ejection fraction: a simple parameter to predict long-term mortality
DOI:
https://doi.org/10.47487/apcyccv.v6i2.466Keywords:
Heart Failure, Prognosis, Pulmonary HypertensionAbstract
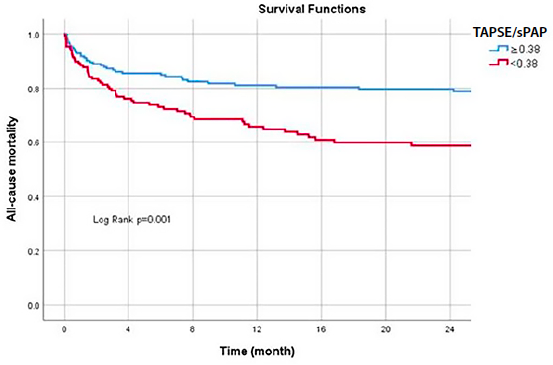
Introduction. Risk prediction in acute heart failure (AHF) has led to the development of multiple prognostic models. Emerging data highlight the prognostic significance of right ventricular (RV) to pulmonary artery (PA) uncoupling, which has been linked to adverse outcomes. Among patients with heart failure with preserved ejection fraction (HFpEF) and mildly reduced ejection fraction (HFmrEF), a highly heterogeneous group, the prognostic relevance of RV-PA uncoupling in forecasting longterm mortality is still not well defined. This study aimed to evaluate the association between RV-PA uncoupling and long-term mortality in a cohort of hospitalized HFpEF and HFmrEF patients. Materials and Methods. We performed a retrospective analysis based on a prospective registry of adult patients admitted with a primary diagnosis of AHF between 2015 and 2020. Eligible patients had a left ventricular ejection fraction (LVEF) > 40%. The main outcome was all-cause mortality over long-term follow-up. RV-PA coupling was quantified using the ratio between tricuspid annular plane systolic excursion (TAPSE) and systolic pulmonary artery pressure (sPAP). Results. Out of 465 patients, simultaneous estimation of TAPSE and sPAP was feasible in 361 cases (77%). During a median follow-up of 20.9 months, 100 patients (27.7%) died. A TAPSE/sPAP ratio of 0.38 was identified as the optimal cut-off for risk discrimination. Notably, 41.8% of patients had values below this threshold. Multivariable analysis confirmed that RV-PA uncoupling (TAPSE/sPAP < 0.38) was independently associated with increased long-term mortality (HR: 2.21; 95% CI 1.26–3.81; P = 0.005). Conclusion. In patients hospitalized for AHF with preserved and mildly reduced ejection fraction, RV-PA uncoupling, as determined by the TAPSE/sPAP ratio, was independently associated with long-term all-cause mortality. This echocardiographic parameter may help identify a subgroup of patients at higher risk during follow-up.
Downloads
References
Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8(1):30-41. doi: 10.1038/ nrcardio.2010.165.
Cleland J. National Heart Failure Audit: April2011 to March 2012. National Institute for Cardiovascular Outcomes Research (NICOR), The Institute of Cardiovascular Science. London: University College, 2012.
Ketchum ES, Levy WC. Establishing prognosis in heart failure: a multimarker approach. Prog Cardiovasc Dis. 2011;54(2):86-96. doi: 10.1016/j.pcad.2011.03.003.
Allen LA, Stevenson LW, Grady KL, Goldstein NE, Matlock DD, Arnold RM, et al. Decision making in advanced heart failure: a scientific statement from the American Heart Association. Circulation. 2012;125(15):1928-52. doi: 10.1161/CIR.0b013e31824f2173.
Passantino A, Monitillo F, Iacoviello M, Scrutinio D. Predicting mortality in patients with acute heart failure: Role of risk scores. World J Cardiol. 2015;7(12): 902-911. doi: 10.4330/wjc.v7.i12.902.
Gorter TM, Van Veldhuisen DJ, Bauersachs J, Borlaug BA, Celutkiene J, Coats AJS, et al. Right heart dysfunction and failure in heart failure with preserved ejection fraction: mechanisms and management. Position statement on behalf of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018;20(1):16-37. doi: 10.1002/ejhf.1029.
Ghio S, Gavazzi A, Campana C, Inserra C, Klersy C, Sebastiani R, Arbustini E, et al. Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol. 2001;37(1):183- 8. doi: 10.1016/s0735-1097(00)01102-5.
Gorter TM, Hoendermis ES, van Veldhuisen DJ, Voors AA, Lam CS, Geelhoed B, et al. Right ventricular dysfunction in heart failure with preserved ejection fraction: a systematic review and meta-analysis. Eur J Heart Fail. 2016;18(12):1472-1487. doi: 10.1002/ejhf.630.
Melenovsky V, Hwang SJ, Lin G, Redfield MM, Borlaug BA. Right heart dysfunction in heart failure with preserved ejection fraction. Eur Heart J. 2014;35(48):3452-62. doi: 10.1093/eurheartj/ehu193.
Guazzi M, Bandera F, Pelissero G, Castelvecchio S, Menicanti L, Ghio S, et al. Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: an index of right ventricular contractile function and prognosis. Am J Physiol Heart Circ Physiol. 2013;305(9):H1373-81. doi: 10.1152/ajpheart.00157.2013.
Guazzi M, Dixon D, Labate V, Beussink-Nelson L, Bandera F, Cuttica MJ, et al. RV Contractile Function and its Coupling to Pulmonary Circulation in Heart Failure With Preserved Ejection Fraction. JACC Cardiovasc Imaging. 2017;10(10 Pt B):1211-1221. doi: 10.1016/j. jcmg.2016.12.024.
Santas E, Palau P, Guazzi M, Espriella R, Miñana G, Sanchis J, et al. Usefulness of Right Ventricular to Pulmonary Circulation Coupling as an Indicator of Risk for Recurrent Admissions in Heart Failure With Preserved Ejection Fraction. Am J Cardiol. 2019;124(4):567-572. doi: 10.1016/j.amjcard.2019.05.024.
Pestelli G, Fiorencis A, Trevisan F, Luisi GA, Smarrazzo V, Mele D. New measures of right ventricle-pulmonary artery coupling in heart failure: An all-cause mortality echocardiographic study. Int J Cardiol. 2021;329:234-241. doi: 10.1016/j.ijcard.2020.12.057.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1-39.e14. doi: 10.1016/j. echo.2014.10.003.
Sciomer S, Magri D, Badagliacca R. Non-invasive assessment of pulmonary hypertension: Doppler-echocardiography. Pulm Pharmacol Ther. 2007;20(2):135-40. doi: 10.1016/j.pupt.2006.03.008.
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23(7):685-713; quiz 786-8. doi: 10.1016/j. echo.2010.05.010. PMID: 20620859.
Nakagawa A, Yasumura Y, Yoshida C, Okumura T, Tateishi J, Yoshida J, et al. Prognostic Importance of Right Ventricular-Vascular Uncoupling in Acute Decompensated Heart Failure With Preserved Ejection Fraction. Circ Cardiovasc Imaging. 2020;13(11):e011430. doi: 10.1161/ CIRCIMAGING.120.011430.
Roh J, Hill JA, Singh A, Valero-Muñoz M, Sam F. Heart Failure With Preserved Ejection Fraction: Heterogeneous Syndrome, Diverse Preclinical Models. Circ Res. 2022;130(12):1906-1925. doi: 10.1161/ CIRCRESAHA.122.320257.
Shah SJ, Katz DH, Deo RC. Phenotypic spectrum of heart failure with preserved ejection fraction. Heart Fail Clin. 2014;10(3):407-18. doi: 10.1016/j.hfc.2014.04.008.
Obokata M, Reddy YNV, Melenovsky V, Pislaru S, Borlaug BA. Deterioration in right ventricular structure and function over time in patients with heart failure and preserved ejection fraction. Eur Heart J. 2019;40(8):689-697. doi: 10.1093/eurheartj/ehy809.
Guazzi M, Naeije R. Pulmonary hypertension in heart failure: pathophysiology, pathobiology, and emerging clinical perspectives. J Am Coll Cardiol. 2017;69(13):1718-1734. doi: 10.1016/j. jacc.2017.01.051.
Jang AY, Park SJ, Chung WJ. Pulmonary hypertension in heart failure. Int J Heart Fail. 2021;3(3):147-159. doi: 10.36628/ijhf.2020.0053.
Kim BJ, Kim SJ, Im SI, Kim HS, Heo JH, Shin HS, et al. Increased right ventricular pressure as a predictor of acute decompensated heart failure in end-stage renal disease patients on maintenance hemodialysis. Int J Heart Fail. 2022;4(3):154-162. doi: 10.36628/ ijhf.2022.0001.
Monitillo F, Di Terlizzi V, Gioia MI, Barone R, Grande D, Parisi G, et al. Right ventricular function in chronic heart failure: from the diagnosis to the therapeutic approach. J Cardiovasc Dev Dis. 2020;7(2):12. doi: 10.3390/jcdd7020012.
He Q, Lin Y, Zhu Y, Gao L, Ji M, Zhang L, Xie M, Li Y. Clinical Usefulness of Right Ventricle-Pulmonary Artery Coupling in Cardiovascular Disease. J Clin Med. 2023;12(7):2526. doi: 10.3390/jcm12072526.
Naseem M, Alkassas A, Alaarag A. Tricuspid annular plane systolic excursion/pulmonary arterial systolic pressure ratio as a predictor of in-hospital mortality for acute heart failure. BMC Cardiovasc Disord. 2022;22(1):414. doi: 10.1186/s12872-022-02857-6.
Bonelli A, Pagnesi M, Inciardi RM, Castiello A, Sciatti E, Carubelli V, et al. Prognostic role of tricuspid annular plane systolic excursion/ pulmonary artery systolic pressure ratio in patients hospitalized for acute heart failure. J Cardiovasc Med (Hagerstown). 2023;24(8):564- 574. doi: 10.2459/JCM.0000000000001499.
Fauvel C, Dillinger JG, Rossanaly Vasram R, Bouleti C, Logeart D, et al. ADDICT-ICCU Investigators. In-hospital Prognostic Value of TAPSE/sPAP in Patients Hospitalized for Acute Heart Failure. Eur Heart J Cardiovasc Imaging. 2024;25(8):1099-1108. doi: 10.1093/ehjci/jeae059.
Bok Y, Kim JY, Park JH. Prognostic Role of Right Ventricular-Pulmonary Artery Coupling Assessed by TAPSE/PASP Ratio in Patients With Acute Heart Failure. J Cardiovasc Imaging. 2023;31(4):200-206. doi: 10.4250/jcvi.2023.0055.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














