Clinical predictors of coronary artery bypass graft surgery in patients hospitalized for Non-ST acute coronary syndrome - Buenos Aires I and ReSCAR22 registries
DOI:
https://doi.org/10.47487/apcyccv.v5i1.333Keywords:
Myocardial Revascularization, Coronary Artery Disease, Acute Coronary Syndrome, ArgentinaAbstract
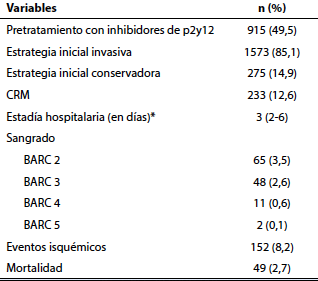
Objectives. To identify predictors of coronary artery bypass graft surgery (CABG) requirement as a revascularization method in in real-world non-ST-segment elevation acute coronary syndrome (NSTE-ACS) patients. Materials and methods. An individual pre-specified analysis of patients with NSTE-ACS was performed from two prospective Argentine registries between 2017 and 2022. We analyzed the difference in baseline characteristics between patients who required CABG and those who did not require this intervention. Then, a logistic regression analysis was performed to determine independent predictors in patients who received CABG as a method of revascularization. Results. A total of 1848 patients with a median age of 54.8 (interquartile range [IQR]: 53.7-56) years and an ejection fraction of 42.1% (IQR: 41.2-43.1) were included. A total of 233 patients required CABG (12.6%). Baseline characteristics between the two groups were similar, except in patients requiring CABG, who were younger (51.5 vs. 55.7 years; p=0.010), more frequently diabetic (38.2% vs. 25.7%; p=0.001) and male (90.1% vs. 73.7%; p=0.001). In addition, they had, to a lesser extent, previous cardiac surgery (2.1% vs. 11.2%; p=0.011). After multivariable analysis, the following were independently associated with CABG: age (Odds Ratio [OR]: 0.99, 95% confidence interval [CI]: 0.98-0.99; p=0.008), male sex (OR: 3.08, 95% CI: 1.87-5.1; p=0.001), history of previous CABG (OR: 0.14, 95% CI: 0.05-0.30; p=0.001) and diabetes (OR: 1.84, 95% CI: 1.31- 2.57; p=0.001). Conclusions. In this analysis of two NSTEACS registries, younger age, male sex, a diagnosis of diabetes and the absence of previous surgery were independent predictors of the requirement for inpatient CABG.
Downloads
References
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. EuroIntervention. 2019;14(14):1435-1534. doi: 10.4244/EIJY19M01_01.
Lawton JS, Tamis-Holland JE, Bangalore S, Bates ER, Beckie TM, Bischoff JM, et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(3):e4-e17. doi: 10.1161/CIR.0000000000001039.
Gaudino M, Hameed I, Farkouh ME, Rahouma M, Naik A, Robinson NB, et al. Overall and Cause-Specific Mortality in Randomized Clinical Trials Comparing Percutaneous Interventions With Coronary Bypass Surgery: A Meta-analysis. JAMA Intern Med. 2020;180(12):1638-1646. doi: 10.1001/jamainternmed.2020.4748.
Palm DS, Drame A, Moliterno DJ, Aguilar D. Acute Coronary Syndromes Among Patients with Prior Coronary Artery Bypass Surgery. Curr Cardiol Rep. 2022;24(11):1755-1763. doi: 10.1007/ s11886-022-01784-4.
Ram E, Sternik L, Moshkovitz Y, Iakobishvili Z, Zuroff E, Peled Y, et al. Coronary Artery Bypass Grafting Following Acute Coronary Syndrome: Impact of Gender. Semin Thorac Cardiovasc Surg. 2022;34(3):920–9. doi: 10.1053/j.semtcvs.2021.07.015.
Godoy LC, Lawler PR, Farkouh ME, Hersen B, Nicolau JC, Rao V. Urgent Revascularization Strategies in Patients With Diabetes Mellitus and Acute Coronary Syndrome. Can J Cardiol. 2019;35(8):993-1001. doi: 10.1016/j.cjca.2019.03.010.
Hadaya J, Sanaiha Y, Tran Z, Downey P, Shemin RJ, Benharash P. Timing of Coronary Artery Bypass Grafting in Acute Coronary Syndrome: A National Analysis. Ann Thorac Surg. 2022;113(5):1482- 1490. doi: 10.1016/j.athoracsur.2021.05.057.
Hwang B, Williams ML, Tian DH, Yan TD, Misfeld M. Coronary artery bypass surgery for acute coronary syndrome: A network meta- analysis of on-pump cardioplegic arrest, off-pump, and on-pump beating heart strategies. J Card Surg. 2022;37(12):5290-5299. doi: 10.1111/jocs.17149.
Costabel JP, Zaidel E, Rivero M, Gomez I, Perez G. Registro multicéntrico prospectivo de pacientes hospitalizados por síndrome coronario agudo sin elevación del segmento ST en centros de alta complejidad. Resultados intrahospitalarios y evolución a 6 meses (Buenos Aires I). Rev argent cardiol. 2020;88(4):308-16. doi: 10.7775/ rac.es.v88.i4.18501.
Rivero M, Feder J, Procopio G, Gingins M, Souto JM, Villarreal R, et al. Registro de síndromes coronarios agudos en centros de alta complejidad de Argentina. ReSCAR 2022. Rev Argent Cardiol. 2023;91:205-11. doi: 10.7775/rac.es.v91.i3.20631.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138(20):e618-e651. doi: 10.1161/ CIR.0000000000000617.
Fox KA, Eagle KA, Gore JM, Steg PG, Anderson FA; GRACE and GRACE2 Investigators. The Global Registry of Acute Coronary Events, 1999 to 2009--GRACE. Heart. 2010;96(14):1095-101. doi: 10.1136/hrt.2009.190827.
Carvalho JF, Belo A, Congo K, Neves D, Santos AR, Piçarra B, et al. Left main and/or three-vessel disease in patients with non-ST- segment elevation myocardial infarction and low-risk GRACE score: Prevalence, clinical outcomes and predictors. Rev Port Cardiol (Engl Ed). 2018;37(11):911-919. doi: 10.1016/j.repc.2018.03.016.
Fox KA, Steg PG, Eagle KA, Goodman SG, Anderson FA Jr, Granger CB, et al. Decline in rates of death and heart failure in acute coronary syndromes, 1999-2006. JAMA. 2007;297(17):1892-900. doi: 10.1001/jama.297.17.1892.
SmilowitzNR,MahajanAM,RoeMT,HellkampAS,ChiswellK,GulatiM, et al. Mortality of Myocardial Infarction by Sex, Age, and Obstructive Coronary Artery Disease Status in the ACTION Registry-GWTG (Acute Coronary Treatment and Intervention Outcomes Network Registry-Get With the Guidelines). Circ Cardiovasc Qual Outcomes. 2017;10(12):e003443. doi: 10.1161/CIRCOUTCOMES.116.003443.
Porter A, Paradkar A, Goldenberg I, Shlomo N, Cohen T, Kornowski R, et al. Temporal Trends Analysis of the Characteristics, Management, and Outcomes of Women With Acute Coronary Syndrome (ACS): ACS Israeli Survey Registry 2000-2016. J Am Heart Assoc. 2020;9(1):e014721. doi: 10.1161/JAHA.119.014721.
Farooq V, Van Klaveren D, Steyerberg EW, Meliga E, Vergouwe Y, Chieffo A, et al. Anatomical and clinical characteristics to guide decision making between coronary artery bypass surgery and percutaneous coronary intervention for individual patients: Development and validation of SYNTAX score II. The Lancet. 2013;381(9867):639-50. doi: 10.1016/S0140-6736(13)60108-7.
Wang R, Tomaniak M, Takahashi K, Gao C, Kawashima H, Hara H, et al. Impact of chronic obstructive pulmonary disease on 10-year mortality after percutaneous coronary intervention and bypass surgery for complex coronary artery disease: insights from the SYNTAX Extended Survival study. Clin Res Cardiol. 2021;110(7):1083- 1095. doi: 10.1007/s00392-021-01833-y.
Ono M, Serruys PW, Hara H, Kawashima H, Gao C, Wang R, et al. 10-Year Follow-Up After Revascularization in Elderly Patients With Complex Coronary Artery Disease. J Am Coll Cardiol. 2021;77(22):2761-2773. doi: 10.1016/j.jacc.2021.04.016.
Tesauro M, Mauriello A, Rovella V, Annicchiarico-Petruzzelli M, Cardillo C, Melino G, et al. Arterial ageing: from endothelial dysfunction to vascular calcification. J Intern Med. 2017;281(5):471- 482. doi: 10.1111/joim.12605.
Farkouh ME, Domanski M, Dangas GD, Godoy LC, Mack MJ, Siami FS, et al. Long-Term Survival Following Multivessel Revascularization in Patients With Diabetes: The FREEDOM Follow-On Study. J Am Coll Cardiol. 2019;73(6):629-638. doi: 10.1016/j.jacc.2018.11.001.
Kapur A, Hall RJ, Malik IS, Qureshi AC, Butts J, de Belder M, et al. Randomized comparison of percutaneous coronary intervention with coronary artery bypass grafting in diabetic patients. 1-year results of the CARDia (Coronary Artery Revascularization in Diabetes) trial. J Am Coll Cardiol. 2010;55(5):432-40. doi: 10.1016/j. jacc.2009.10.014.
Mamet H, Petrie MC, Rocchiccioli P. Type 1 diabetes mellitus and coronary revascularization. Cardiovasc Endocrinol Metab. 2019;8(1):35-38. doi: 10.1097/XCE.0000000000000166.
FarkouhME,DomanskiM,SleeperLA,SiamiFS,DangasG,MackM, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012 Dec;367(25):2375-84. doi: 10.1056/ NEJMoa1211585.
Gholap NN, Achana FA, Davies MJ, Ray KK, Gray L, Khunti K. Long- term mortality after acute myocardial infarction among individuals with and without diabetes: A systematic review and meta-analysis of studies in the post-reperfusion era. Diabetes Obes Metab. 2017;19(3):364-374. doi: 10.1111/dom.12827.
HeadSJ,DavierwalaPM,SerruysPW,RedwoodSR,ColomboA,Mack MJ, et al. Coronary artery bypass grafting vs. percutaneous coronary intervention for patients with three-vessel disease: final five-year follow-up of the SYNTAX trial. Eur Heart J. 2014;35(40):2821-30. doi: 10.1093/eurheartj/ehu213.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














