Impact of a multidisciplinary team “ECMO Team” on the prognosis of patients undergoing veno-arterial extracorporeal membrane oxygenation for refractory cardiogenic shock and cardiac arrest
DOI:
https://doi.org/10.47487/apcyccv.v4i4.325Keywords:
Heart Arrest, Patient Care Team, Extracorporeal Membrane Oxygenation, Shock, CardiogenicAbstract
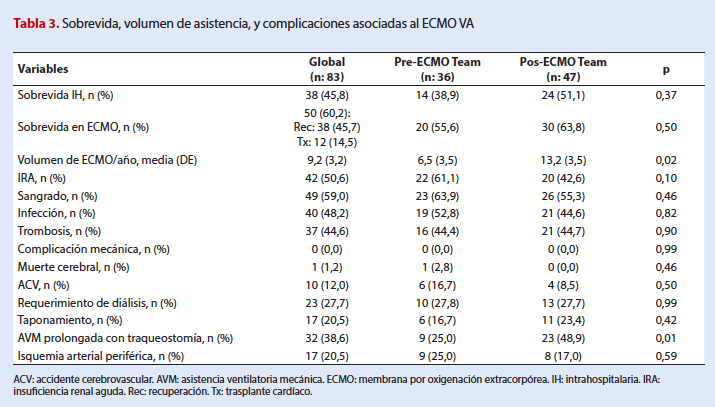
Objectives. Veno-arterial Extracorporeal membrane oxygenation (VA ECMO) is a salvage intervention in patients with cardiogenic shock (CS), and cardiac arrest (CA) refractory to standard therapies. The design of ECMO Teams has achieved the standardization of processes, although its impact on survival and prognosis is unknown. Objective: We aimed to analyze whether the creation of an ECMO Team has modified the prognosis of patients undergoing VA ECMO for refractory CS or CA. Materials and methods. We conducted a single-center retrospective cohort study. Patients with refractory CS or CA who underwent VA ECMO were divided in two consecutive periods: from 2014 to April 2019 (pre-ECMO T) and from May 2019 to December 2022 (Post ECMO T). The main outcomes were survival on ECMO, in-hospital survival, complications, and annual ECMO volume. Results. Eighty-three patients were included (36 pre-ECMO T and 47 post-ECMO T). The mean age was 53 +/-13 years. The most common reason for device indication was different: postcardiotomy shock (47.2%) pre-ECMO T and refractory cardiogenic shock (29.7%) post-ECMO T. The rate of extracorporeal cardiopulmonary resuscitation was 14.5%. The median duration of VA ECMO was longer after ECMO team implementation: 8 days (IQR 5-12.5) vs. five days (IQR 2-9, p=0.04). Global in-hospital survival was 45.8% (38.9% pre-ECMO T vs. 51.1% post-ECMO T; p=0.37), and the survival rate from VA ECMO was 60.2% (55.6% pre-ECMO T vs 63.8% post-ECMO T; p= 0.50). The volume of VA ECMO implantation was significantly higher in the post-ECMO team period (13.2 +/3.5 per year vs. 6.5 +/-3.5 per year, p: 0.02). The rate of complications was similar in both groups. Conclusions. After the implementation of an ECMO team, there was no statistical difference in the survival rate of patients treated with VA ECMO. However, a significant increase in the number of patients supported per year was observed after the implementation of this multidisciplinary team. Post-ECMO T, the most common reason for device indication was cardiogenic shock, with longer run times and a higher rate of extracorporeal cardiopulmonary resuscitation.
Downloads
References
Makdisi G, Wang I. Extra corporeal membrane oxygenation (ECMO) review of a lifesaving technology. J Thorac Dis. 2015;7(7):166-76. doi: 10.3978/j.issn.2072-1439.2015.07.17.
Barbaro RP, Odetola FO, Kidwell KM, Paden ML, Bartlett RH, Davis MM, et al. Association of hospital-level volume of extracorporeal membrane oxygenation cases and mortality. Analysis of the extracorporeal life support organization registry. Am J Respir Crit Care Med. 2015;191(8):894-901. doi: 10.1164/rccm.201409-1634OC.
Extracorporeal Life Support Organization (ELSO). ELSO Guidelines for ECMO Centers, Extracorporeal Life Support Organization [Internet]. Ann Arbor, MI: ELSO; 2017 [citado el 7 de julio de 2023]. Disponible en: https://www.elso.org/ecmo-resources/elso-ecmo-guidelines.aspx
Extracorporeal Life Support Organization (ELSO). ELSO Registry [Internet]. Ann Arbor, MI: ELSO; 2017 [citado el 12 de agosto de 2023]. Disponible en: https://www.elso.org/registry/internationalsummaryandreports/internationalsummary.aspx
DellaVolpe J, Barbaro RP, Cannon JW, Fan E, Greene WR, Gunnerson KJ, et al. Joint Society of Critical Care Medicine-Extracorporeal Life Support Organization Task Force Position Paper on the role of the intensivist in the initiation and management of extracorporeal membrane oxygenation. Crit Care Med. 2020;48(6):838-46. doi: 10.1097/CCM.0000000000004330.
Dalia AA, Ortoleva J, Fiedler A, Villavicencio M, Shelton K, Cudemus GD. ECMO is a Team sport: Institutional Survival benefits of a formalized ECMO Team. J Cardiothorac Vasc Anesth. 2019;33(4):902-7. doi: 10.1053/j.jvca.2018.06.003.
Goh KJ, Tan QL, Tay CK, Sewa DW, Hooi Lee KC, Phua GC. Impact of an Extracorporeal Membrane Oxygenation intensivist-Led multidisciplinary team on venovenous extracorporeal membrane oxygenation outcomes. Crit Care Explor. 2020;2(12):e0297. doi: 10.1097/CCE.0000000000000297.
Na SJ, Chung CR, Choi HJ, Cho YH, Sung K, Yang JH, et al. The effect of multidisciplinary extracorporeal membrane oxygenation team on clinical outcomes in patients with severe acute respiratory failure. Ann intensive care. 2018;8(1):31. doi: 10.1186/s13613-018-0375-9.
Komindr A, Abe R, Tateishi Y, Takahashi Y, Goto J, Wada K, et al. Establishing extracorporeal membrane oxygenation team increased number of patients and improved data recording. J Intensive Care. 2019;7:11. doi: 10.1186/s40560-019-0366-4. eCollection 2019.
Cotza M, Carboni G, Ballotta A, Kandil H, Isgró G, Carlucci C, et al. Modern ECMO: why an ECMO programme in a tertiary care hospital. Eur Heart J Supp. 2016;18(Suppl E):79-85. doi: 10.1093/eurheartj/suw016.
Barbaro RP, Odetola FO, Kidwell KM, Paden ML, Bartlett RH, Davis MM, et al. Association of hospital-level volume of extracorporeal membrane oxygenation cases and mortality. Analysis of the extracorporeal life support organization registry. Am J Respir Crit Care Med. 2015;191(8):894-901. doi: 10.1164/rccm.201409-1634OC.
Tchantchaleishvili V, Hallinan W, Massey HT. Call for Organized Statewide Networks for Management of Acute Myocardial Infarction-Related Cardiogenic Shock. JAMA Surg. 2015;150(11):1025-6. doi: 10.1001/jamasurg.2015.2412.
Doll JA, Ohman EM, Patel MR, Milano CA, Rogers JG, Wohns DH, et al. A team‐based approach to patients in cardiogenic shock. Catheter Cardiovasc Interv. 2016;88(3):424-33. doi: 10.1002/ccd.26297.
Tehrani BN, Truesdell AG, Sherwood MW, Desai S, Tran HA, Epps KC, et al. Standardized team‐based care for cardiogenic shock. J Am Coll Cardiol. 2019;73(13):1659-1669. doi: 10.1016/j.jacc.2018.12.084.
Lee F, Hutson JH, Boodhwani M, McDonald B, So D, de Roock S, et al. Multidisciplinary code shock team in cardiogenic shock: a Canadian‐center experience. CJC Open. 2020;2(4):249-257. doi: 10.1016/j.cjco.2020.03.009.
Moghaddam N, van Diepen S, So D, Lawler PR, Fordyce CB. Cardiogenic shock teams and centres: a contemporary review of multidisciplinary care for cardiogenic shock. ESC Heart Fail. 2021;8(2):988-98. doi: 10.1002/ehf2.13180.
Taleb I, Koliopoulou AG, Tandar A, McKellar SH, Tonna JE, Nativi-Nicolau J, et al. Shock team approach in refractory cardiogenic shock requiring short-term mechanical circulatory support. Circulation. 2019;140(1):98-100. doi: 10.1161/CIRCULATIONAHA.119.040654.
Moll V, Teo EYL, Grenda DS, Powell CD, Connor Jr MJ, Gartland BT, et al. Rapid development and implementation of an ECMO program. ASAIO J. 2016;62(3):354-8. doi: 10.1097/MAT.0000000000000331.
Nagaoka E, Arai H, Ugawa T, Masuda T, Ochiai K, Tamaoka M, et al. Efficacy of multidisciplinary team approach with extracorporeal membrane oxygenation for COVID-19 in a low volume ECMO center. Artif Organs. 2021;45(9):1061-7. doi: 10.1111/aor.13947.
Assy J, Skouri H, Charafeddine L, Majdalani M, Younes K, Bulbul Z, et al. Establishing an ECMO program in a developing country: challenges and lessons learned. Perfusion. 2019;34(6):508-15. doi: 10.1177/0267659119834489.
Downloads
Published
Issue
Section
License
Copyright (c) 2023 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














