Effectiveness of tertiary prevention on quality of life and control of risk factors in patients with ischemic coronary heart disease
DOI:
https://doi.org/10.47487/apcyccv.v4i3.323Keywords:
Tertiary Prevention, Cardiac Rehabilitation, Quality of Life, Heart Disease Risk FactorsAbstract
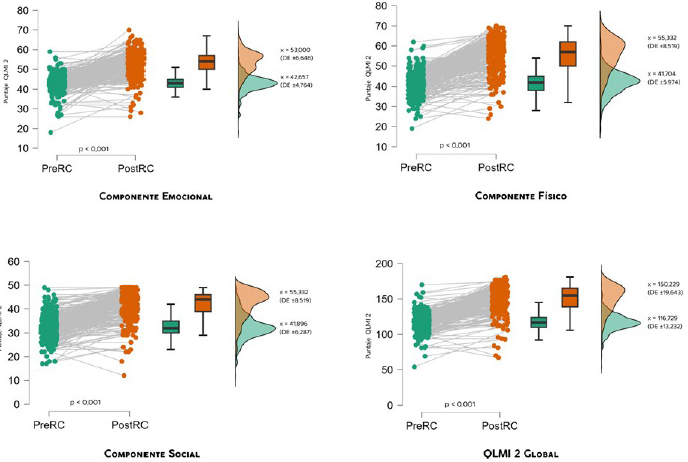
Objective. Determine the effectiveness of cardiac rehabilitation (CR) as a tertiary prevention strategy in the quality of life and control of risk factors of patients with ischemic coronary heart disease (ICC) of the National Cardiovascular Institute (INCOR) of EsSalud- Lima during the year 2018. Materials and methods. A retrospective cohort of 280 patients with a diagnosis of CCI was studied who, after medical, interventional, or surgical treatment, were referred to the INCOR CR program for tertiary prevention (PT) in 2018. The program was developed according to the institutional guide for eight weeks with exercise sessions and educational, psychological, nutritional, and recreational workshops. At the beginning and at the end of this, the QLMI-2 quality of life test was applied, and anthropometric, laboratory, and risk factor control measurements were performed. Results. Quality of life levels at the end of CR showed a statistically significant improvement in the emotional, social, physical, and global dimensions (p < 0.001). The same behavior was observed for the nutritional variables of weight, abdominal circumference, and BMI (p < 0.001). Physical capacity showed a statistically significant improvement in the aspects of muscle strength (12.2%), physical activity (38.0%), and functional capability (25.4%) (p < 0.001). The result was not homogeneous for the biochemical metabolic variables, where glycosylated hemoglobin, glycemia, and lipid profile did not show significant improvement, except for HDL, which raised its levels statistically significantly (p < 0.001). Conclusions. CR is effective as a central strategy to perform tertiary prevention in patients with ICC since it notably improves quality of life and coronary risk factors.
Downloads
References
Wang F, Yu Y, Mubarik S, Zhang Y, Liu X, Cheng Y, et al. Global Burden of Ischemic Heart Disease and Attributable Risk Factors, 1990-2017: A Secondary Analysis Based on the Global Burden of Disease Study
Clin Epidemiol. 2021;13:859-870. doi: 10.2147/CLEP.S317787.
Murray CJL. The global burden of disease study at 30 years. Nat Med. 2022;28(10):2019-2026. doi: 10.1038/s41591-022-01990-1.
Segura Vega L, Agusti R, Ruiz Mori E, Investigadores Tornasol II. La hipertensión arterial en el Perú según el estudio TORNASOL II. Rev Peru Cardiol. 2011;37(1):19-27.
Centro Nacional de Epidemiología, Prevención y Control de Enfermedades. Estudio de Carga de Enfermedad [Internet]. Lima, Perú: Ministerio de Salud; c2023 [citado 7 de abril de 2023]. Disponible en: https://www.dge.gob.pe/portalnuevo/inteligenciasanitaria/carga-de-enfermedad-y-analisis-de-la-demanda/
Centro Nacional de Epidemiología, Prevención y Control de Enfermedades, Ministerio de Salud. Análisis de Situación de Salud del Perú, 2021. Lima, Perú: Ministerio de Salud; 2023.
Instituto de Evaluación de Tecnologías en Salud e Investigación - IETSI. Guía de práctica clínica para el manejo de la Hipertensión Arterial Esencial [Internet]. Lima, Perú: Seguro Social de Salud - EsSalud; 2022 [citado 7 de abril de 2023]. Disponible en: https://gpc-peru.com/hipertension
Araújo O, Ardanaz N, Bachman R, Bianco E, Burdiat G, Díaz Arnesto O, et al. Guía práctica de prevención cardiovascular. Rev Urug Cardiol. 2009;24(1):43-83.
Vegas-Valle JM, García-Ruiz JM, Hernández-Martín E, De La Hera JM. Síndrome metabólico, diabetes y enfermedad coronaria: Una relación muy frecuente. Rev Esp Cardiol. 2012;65(1):108-9. doi: 10.1016/j.recesp.2011.07.006.
Arocha Rodulfo JI. Aproximación al continuo cardiometabólico. descripción narrativa. Clín Investig Arterioscler. 2021;33(3):158-67. doi: 10.1016/j.arteri.2020.10.003.
Moya RRM, Ros ÁL, Al-Mahdi EAR, Gómez JLZ. Prevención y tratamiento de los factores de riesgo cardiovascular. Medicine. 2021;13(36):2081-8. doi: 10.1016/j.med.2021.06.012.
Leavell HR, Clark EG. Textbook of preventive medicine. McGraw-Hill, New York, 1953.
Arouca S. La historia natural de las enfermedades. Rev Cubana de Salud Pública. 2018;44(4):220-8.
Sarver Heart Center. 10 Consejos para prevenir enfermedades del corazón y accidente cerebrovascular (apoplejía o derrame cerebral) [Internet]. Tucson, AZ: The University of Arizona; 2021 [citado 27 de abril de 2023]. Disponible en: https://heart.arizona.edu/heart-health/informaci%C3%B3n-en-espa%C3%B1ol/10-consejos-para-prevenirenfermedades-del-coraz%C3%B3n-y-accidente
Niebauer J. Cardiac Rehabilitation Manual. London: Springer Cham; 2017.
Torres MMM, Moreira GAC, Bailón XTS, Anchundia JJP, Castro YXA, Zambrano CFS. Riesgo cardiovascular y rehabilitación cardíaca de pacientes cardiópatas. RECIMUNDO. 2020;4(1):442-52. doi: 10.26820/recimundo/4.(1).enero.2020.442-452.
Cano de la Cuerda R, Alguacil Diego IM, Alonso Martín JJ, Molero Sánchez A, Miangolarra Pagea JC. Programas de rehabilitación cardíaca y calidad de vida relacionada con la salud: Situación actual. Rev Urug Cardiol. 2013;28(2):258-258.
Instituto de Evaluación de Tecnologías en Salud e Investigación. Guía de práctica clínica de rehabilitación cardiaca. Lima, Perú: EsSalud; 2018.
Brotons Cuixart C, Ribera Solé A, Permanyer Miralda G, Cascant Castelló P, Moral Peláez I, Pinar Sopena J, et al. Adaptación del cuestionario de calidad de vida postinfarto MacNew OLMI para su uso en la población española. Med Clin. 2000;115(20):768-71. doi: 10.1016/S0025-7753(00)71687-3.
Hernández Sampieri R, Fernández Collado C, Baptista Lucio P. Metodología de la investigación [Internet]. Vol. 4. México: McGraw-Hill Interamericana; 2018 [citado 6 de octubre de 2023]. Disponible en: https://www.academia.edu/download/38911499/luis_investigacion.pdf
University of Amsterdam. JASP - A fresh way to do statistics [Internet]. Amsterdam: University of Amsterdam; 2023 [citado 22 de octubre de 2023]. Disponible en: https://jasp-stats.org/
Bjarnason-Wehrens B, McGee H, Zwisler AD, Piepoli MF, Benzer W, Schmid JP, et al. Cardiac rehabilitation in Europe: results from the European Cardiac Rehabilitation Inventory Survey. Eur J Cardiovasc Prev Rehabil. 2010;17(4):410-8. doi: 10.1097/HJR.0b013e328334f42d.
Mark DB, Knight JD, Velazquez EJ, Wasilewski J, Howlett JG, Smith PK, et al. Quality-of-life outcomes with coronary artery bypass graft surgery in ischemic left ventricular dysfunction. Ann Intern Med. 2014;161(6):392-9. doi: 10.7326/M13-1380.
Jiménez Alcántara KM, Pashanase Tello ÁSR. Efectos del programa de prevención secundaria de rehabilitación cardíaca en la capacidad funcional de pacientes varones con cardiopatía coronaria crónica
en un policlínico de Lima Metropolitana en el año 2012-2013 [Internet]. Lima: Universidad Privada Norbert Wiener; 2014 [citado 3 de marzo de 2021]. Disponible en: http://repositorio.uwiener.edu.pe/handle/123456789/94
Apostolopoulou E, Tsagri C, Kipourgos G, Tzenalis A. A study of the biopsychosocial rehabilitation of patients with myocardial infarction six months after their discharge from the cardiac care unit. Health Res J. 2023;9(4):205-18. doi: 10.12681/healthresj.34508.
Rajalakshmi K. The effectiveness of cardiac rehabilitation program to enhance quality of life on patients with post myocardial infarction [Internet]. Gujarat: INFLIBNET Centre; c2023 [citado 14 de octubre de 2023]; Disponible en: https://shodhganga.inflibnet.ac.in:8443/jspui/handle/10603/333417
Da Costa Paiva M, Castro AAM, Ferreira De Carvalho P, Barbosa Sales W, De Oliveira ICS, Neves Mourão M, et al. Effectiveness of cardiac rehabilitation with mHealth through smartphone functionalities: A systematic review protocol. CJC Open [Internet]. 10 de febrero de 2023 [citado 14 de octubre de 2023]. Disponible en: https://www.sciencedirect.com/science/article/pii/S2589790X23000252. doi: 10.1016/j.cjco.2023.02.001.
Casaverde Pineda MF, Escate Quijandría MC, Guerrero León PM. Calidad de vida en pacientes post infarto agudo de miocardio que asisten al Programa de Rehabilitación Cardíaca en un Instituto Nacional 2017 [Internet]. Lima, Perú: Universidad Peruana Cayetano Heredia; 2018 [citado 28 de diciembre de 2018]. Disponible en: https://repositorio.upch.edu.pe/handle/20.500.12866/3762
Anchique Santos CV, Lopez-Jimenez F, Benaim B, Burdiat G, Fernandez Coronado R, Gonzalez G, et al. Cardiac Rehabilitation in Latin America. Prog Cardiovasc Dis. 2014;57(3):268-75. doi: 10.1016/j.pcad.2014.09.006.
Lalonde F. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. J Osteopath Med. 2012;112:753-4. doi: 10.7556/jaoa.2012.112.11.753.
Rivas-Estany E, Barrera-Sarduy JD, Sixto-Fernández S, Rodríguez-Nande LM, Kesser-García C. Programa cubano de rehabilitación cardíaca. Resultados. Rehabilitación (Madr). 2013;47(4):245-8. doi: 10.1016/j.rh.2013.07.003.
Fernández Coronado R. Calidad de la atención y grado de satisfacción del paciente cardíaco transferido de provincia a la consulta externa de cardiología del INCOR 2009 [Internet]. Lima, Perú: Universidad Nacional Mayor de San Marcos; 2009 [citado 26 de diciembre de 2018]. Disponible en: https://cybertesis.unmsm.edu.pe/handle/20.500.12672/3819
Grace SL. Evidence is indisputable that cardiac rehabilitation provides health benefits and event reduction: Time for policy action. Eur Heart J. 2023;44(6):470-2. doi: 10.1093/eurheartj/ehac690.
Mahdavi F, Bagherpoor T, Nemati N. Evaluating the effect of eight weeks of cardiac rehabilitation on functional indices of systolic and diastolic blood pressure, resting heart rate and functional capacity of VO2max and MEt in male patients 55-70 years old with coronary artery bypass graft surgery. Razi J Med Sci. 2023;29(11):233-40.
Kuchmenko O, Tereshchenko N, Malynovska I, Babii L, Shumakov V, Sheiko V, et al. Impact Assessment of Physical Exercise on the factors for progression of atherosclerosis in patients after sustained myocardial infarction: A Three-year follow-up. Zdravotnícke listy [Internet]. 2023 [citado 14 de octubre de 2023];11(2):67-75. Disponible en: https://zl.tnuni.sk/fileadmin/Archiv/2023/2023-11.c.2/ZL_2023_11_2_11_Kuchmenko.pdf
Parhizi F, Rashidlamir A, Khajeie R, Ramezan Pour MR, Vazifedoost M. The effect of a cardiac rehabilitation course on some key factors of reverse cholesterol transfer and TNFα serum level in coronary bypass patients. J Paramed Sci Rehabil [Internet]. 23 de agosto de 2023 [citado 14 de octubre de 2023];12(2). Disponible en: https://jpsr.mums.ac.ir/article_23039_en.html
Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G. Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration (BMI Mediated Effects). Metabolic mediators of the effects of bodymass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of ninety-seven prospective cohorts with 1.8 million participants. Lancet. 2014;383(9921):970-83. doi: 10.1016/S0140-6736(13)61836-X.
Lima de Melo Ghisi G, Pesah E, Turk-Adawi K, Supervia M, Lopez Jimenez F, Grace SL. Cardiac rehabilitation models around the globe. J Clin Med. 2018;7(9):260. doi: 10.3390/jcm7090260.
Turk-Adawi K, Supervia M, Lopez-Jimenez F, Pesah E, Ding R, Britto RR, et al. Cardiac Rehabilitation Availability and Density around the Globe. EClinicalMedicine. 2019;13:31-45. doi: 10.1016/j.eclinm.2019.06.007.
Kellar GG. Cardiac rehabilitation knowledge & attitudes of cardiology fellows [Internet]. Pittsburgh, PA: University of Pittsburgh; 2019 [citado 14 de octubre de 2023]. Disponible en: https://www.proquest.com/docview/2358547538/abstract/7946384DEFED4A04PQ/1
Dahhan A, Maddox WR, Krothapalli S, Farmer M, Shah A, Ford B, et al. Education of physicians and implementation of a formal referral system can improve cardiac rehabilitation referral and participation rates after percutaneous coronary intervention. Heart Lung Circ. 2015;24(8):806-16. doi: 10.1016/j.hlc.2015.02.006.
Zeballos C, Iglesias D, Paz I, Bustamante J, González Naya E, Castiello G, et al. Estado actual de la rehabilitación cardiovascular en argentina. Rev Argent Cardiol. 2021;89(1):37-41. doi: 10.7775/rac.es.v89.i19695.
Cortes-Bergoderi M, Lopez-Jimenez F, Herdy AH, Zeballos C, Anchique C, Santibañez C, et al. Availability and characteristics of cardiovascular rehabilitation programs in south America. J Cardiopulm Rehabil Prev. 2013;33(1):33-41. doi: 10.1097/HCR.0b013e318272153e.
Downloads
Published
Issue
Section
License
Copyright (c) 2023 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














