Arterial lactate levels and their prognostic value in patients undergoing pulmonary thromboendarterectomy
DOI:
https://doi.org/10.47487/apcyccv.v2i2.131Keywords:
Pulmonary hypertension, Pulmonary thromboembolism, Thromboendarterectomy, LactateAbstract
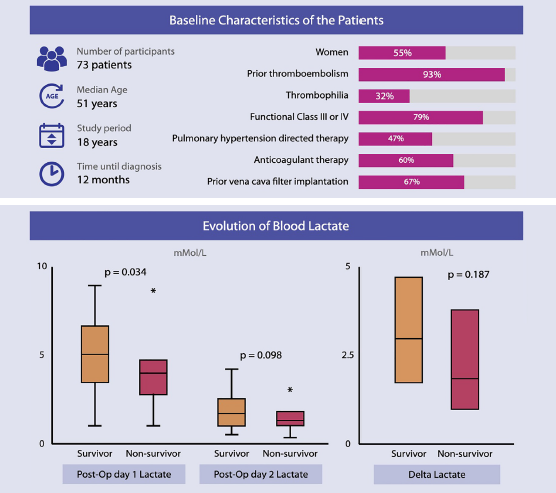
Objective. Evaluate the change of lactate levels and its prognostic role in the postoperative period of patients undergoing pulmonary thromboendarterectomy. Methods. Retrospective study between 2001 and 2019. Patients older than 18 years and who underwent pulmonary thromboendarterectomy were included. The U Mann Whitney test was performed to evaluate the change between lactate levels, and Cox regression analysis to evaluate the relationship with mortality. Areas under the curve were constructed for lactate levels. Results. Seventy-three patients were operated on during the study period. Median age was 51 years, 55% female. The median lactate on days 1 was 4.65 mml/L and on day 2 it was 1.62 mml/L with a change of 2.87 mml/L. No differences were found between the levels measured on day 1 and 2 between the people who died and those who did not on day 30. In the multivariate regression of COX, no relationship with mortality was found. The area under the curve shows regular performance on both day 1 and day 2 in predicting mortality outcomes. Conclusions. The behavior of the lactate in patients undergoing pulmonary thromboendarterectomy shows a rapid change during the first hours after the procedure. No role was found as a predictor of mortality neither in-hospital nor in follow-up.
Downloads
References
Madani MM. Surgical Treatment of Chronic Thromboembolic Pulmonary Hypertension: Pulmonary Thromboendarterectomy. Methodist DeBakey Cardiovasc J. 2016 Dec;12(4):213–8. doi: 10.14797/mdcj-12-4-213.
Riedel M, Stanek V, Widimsky J, et al. Longterm follow-up of patients with pulmonary thromboembolism. Late prognosis and evolution of hemodynamic and respiratory data. Chest. 1982 Feb;81(2):151–8. doi: 10.1378/chest.81.2.151.
Mayer E, Jenkins D, Lindner J, et al. Surgical management and outcome of patients with chronic thromboembolic pulmonary hypertension: results from an international prospective registry. J Thorac Cardiovasc Surg. 2011 Mar;141(3):702–10. doi: 10.1016/j.jtcvs.2010.11.024.
Madani MM, Auger WR, Pretorius V, et al. Pulmonary endarterectomy: recent changes in a single institution’s experience of more than 2,700 patients. Ann Thorac Surg. 2012 Jul;94(1):97–103; discussion 103. doi: 10.1016/j.athoracsur.2012.04.004
Sarkar M, Prabhu V. Basics of cardiopulmonary bypass. Indian J Anaesth. 2017 Sep;61(9):760–7. doi: 10.4103/ija.IJA_379_17
Park SJ, Kim S, Kim JB, et al. Blood lactate level during extracorporeal life support as a surrogate marker for survival. J Thorac Cardiovasc Surg. 2014 Aug;148(2):714–20. doi: 10.1016/j.jtcvs.2014.02.078
Broder G, Weil MH. Excess lactate: an index of reversibility of shock in human patients. Science. 1964 Mar 27;143(3613):1457–9. doi: 10.1126/science.143.3613.1457
Weil MH, Afifi AA. Experimental and clinical studies on lactate and pyruvate as indicators of the severity of acute circulatory failure (shock). Circulation. 1970 Jun;41(6):989–1001. doi: 10.1161/01.cir.41.6.989.
Vincent J-L, De Backer D. Circulatory shock. N Engl J Med. 2013 Oct 31;369(18):1726–34. doi: 10.1056/NEJMra1208943
Nichol AD, Egi M, Pettila V, et al. Relative hyperlactatemia and hospital mortality in critically ill patients: a retrospective multi-centre study. Crit Care Lond Engl. 2010;14(1):R25. doi: 10.1186/cc8888
Haas SA, Lange T, Saugel B, et al. Severe hyperlactatemia, lactate clearance and mortality in unselected critically ill patients. Intensive Care Med. 2016 Feb;42(2):202–10. doi: 10.1007/s00134-015-4127-0
Ranucci M, De Toffol B, Isgrò G, et al. Hyperlactatemia during cardiopulmonary bypass: determinants and impact on postoperative outcome. Crit Care Lond Engl. 2006;10(6):R167. doi: 10.1186/cc5113
Basaran M, Sever K, Kafali E, et al. Serum lactate level has prognostic significance after pediatric cardiac surgery. J Cardiothorac Vasc Anesth. 2006 Feb;20(1):43–7. doi: 10.1053/j.jvca.2004.10.010
Toraman F, Evrenkaya S, Yuce M, et al. Lactic acidosis after cardiac surgery is associated with adverse outcome. Heart Surg Forum. 2004 Apr 1;7(2):E155-159. doi: 10.1532/HSF98.20041002
Khosravani H, Shahpori R, Stelfox HT, et al. Occurrence and adverse effect on outcome of hyperlactatemia in the critically ill. Crit Care Lond Engl. 2009;13(3):R90. doi: 10.1186/cc7918
Warren OJ, Smith AJ, Alexiou C, et al. The inflammatory response to cardiopulmonary bypass: part 1--mechanisms of pathogenesis. J Cardiothorac Vasc Anesth. 2009 Apr;23(2):223–31. doi: 10.1053/j.jvca.2008.08.007
Paparella D, Yau TM, Young E. Cardiopulmonary bypass induced inflammation: pathophysiology and treatment. An update. Eur J Cardio-Thorac Surg Off J Eur Assoc Cardio-Thorac Surg. 2002 Feb;21(2):232–44. doi: 10.1016/s1010-7940(01)01099-5
Kraft F, Schmidt C, Van Aken H, et al. Inflammatory response and extracorporeal circulation. Best Pract Res Clin Anaesthesiol. 2015 Jun;29(2):113–23. doi: 10.1016/j.bpa.2015.03.001
Maillet J-M, Le Besnerais P, Cantoni M, et al. Frequency, risk factors, and outcome of hyperlactatemia after cardiac surgery. Chest. 2003 May;123(5):1361–6. doi: 10.1378/chest.123.5.1361
Demers P, Elkouri S, Martineau R, et al. Outcome with high blood lactate levels during cardiopulmonary bypass in adult cardiac operation. Ann Thorac Surg. 2000 Dec;70(6):2082–6. doi: 10.1016/s0003-4975(00)02160-3
Downloads
Additional Files
Published
Issue
Section
License
Copyright (c) 2021 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














