Five years experience in management of complicated infective endocarditis in a national reference center
DOI:
https://doi.org/10.47487/apcyccv.v1i3.77Keywords:
mortality, endocarditis, complications, blood cultureAbstract
Objective. To evaluate the epidemiological, clinical, echocardiographic, microbiological characteristics and complications of patients with complicated infective endocarditis (IE) in a Peruvian refence hospital.
Material and methods. A retrospective, descriptive study was carried out reviewing the medical records of patients diagnosed with IE treated at Instituto Nacional Cardiovascular-INCOR between years 2012 and 2016; collecting clinical, imaging and laboratory variables.
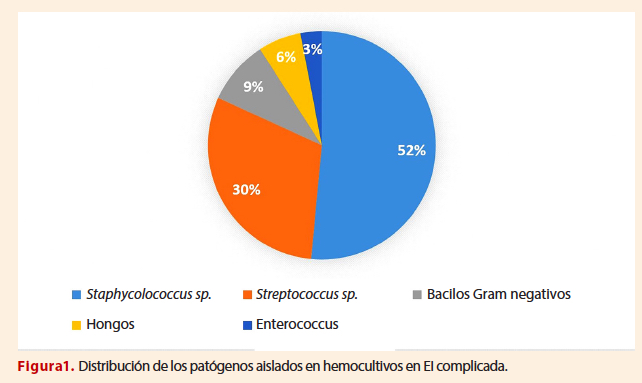
Results. 59 cases were included, predominantly males (66.1%) and the median age was 50 years (IQR 37-62). The most frequent comorbidities were congenital heart disease (42.3%) and the presence of a prosthetic valve (23.7%). The most frequent sign found in the physical examination was fever (69.49%) and the most common symptom was dyspnea (52.5%). The proportion of positive blood cultures was 55.9%, and in 51.5% of these the isolated pathogen was Staphylococcus spp. The most affected valve was the aortic (72.8%), the most frequent finding by echocardiography was the presence of vegetations (91.5%). The most common complications were atrioventricular block (28.8%) and heart failure (22%). Overall, in-hospital mortality was 20.3%.
Conclusion. IE continues to be a challenging pathology, our clinical-epidemiological results are comparable to those found internationally, which reflect the change in the microbiology and in its epidemiology. However, despite advances in diagnosis and treatment, mortality remains unchanged.
Downloads
References
Fedeli U, Schievano E, Buonfrate D, et al. Increasing incidence and mortality of infective endocarditis: a population-based study through a record-linkage system. BMC Infectious Diseases 2011, 11:48.
Toyoda N, Chikwe J, Itagaki S, et al. Trends in infective endocarditis in California and New York State, 1998-2013. JAMA 2017; 317(16):1652-60. DOI:10.1001/jama.2017.4287
Cahill T, Baddour L, Habib G, et al. Challenges in Infective Endocarditis. JACC 2017;69(3):325-44. DOI: http://dx.doi.org/10.1016/j.jacc.2016.10.066
Castillo J, Anguita M, Ruiz M, et al. Cambios epidemiológicos de la endocarditis infecciosa sobre válvula nativa. Rev Esp Cardiol. 2011;64(7):594-98. DOI: 10.1016/j.recesp.2011.03.011
Hubers S, DeSimone D, Bernard J, et al. Infective Endocarditis: A Contemporary Review. Mayo Clin Proc. 2020:1-16. DOI: https://doi.org/10.1016/j.mayocp.2019.12.008.
Habib G, Lancelloti P, Antunes MJ, et al. 2015 ESC Guidelines for management of infective endocarditis: the task forces for the management of infective endocarditis for the European Society of Cardiology. (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36(44):3075-3128. doi:10.1093/eurheartj/ehv319.
Habib G, Erba P, Lung B, et al. Clinical presentation, etiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: a prospective cohort study. Eur Heart J. (2019)0, 1-11.
Avellana P, Garcia M, Swieszkowski S, et al. Endocarditis infecciosa en la República Argentina. Resultados del estudio EIRA 3. Rev Argent Cardiol 2018;86:20-8. http://dx.doi.org/10.7775/rac.es.v86.i1.10935.
Oyonarte M, Montagna R, Braun S. Endocarditis Infecciosa: Experiencia en 506 pacientes del Estudio Cooperativo Nacional en Endocarditis Infecciosa (ECNEI) y sobrevida a 10 años (1998-2008). Rev Chil Cardiol 2008;27(4):(Abstract)-442.
Flores P, Gónzalez P, Berho J, et al. Endocarditis infecciosa: caracterización clínica de la enfermedad. Revisión de casos de los últimos 5 años. Rev Chil Cardiol 2017; 36:34-40
Perez D, Fernández A, Ríos F, et al. Perfil clínico y etiológico de pacientes operados con endocarditis activa. Seguimiento a diez años. Rev Urug Cardiol 2020;35:169-79. DOI: 10.29277/cardio.35.2.8.
Bakir S, Mori T, Durand J, Chen YF, et al. Estrogen-induced vasoprotection is estrogen receptor dependent: evidence from the balloon-injured rat carotid artery model. Circulation 2000; 101(20): 2342-4. DOI:10.1161/01.cir.101.20.2342
Saito C, Padilla M, Valle A, et al. Tratamiento quirúrgico de la endocarditis infecciosa en un hospital general: Indicaciones y morbi-mortalidad. Rev Med Hered. 2014; 25:135-41.
Sanchez E, Gutiérrez C. Evolución y letalidad por endocarditis infecciosa en pacientes atendidos en el Hospital Nacional Dos de Mayo. An Fac Med Lima 2006;67(2):125-33.
Romani F, Cuadra J, Atencia F, et al. Endocarditis infecciosa: análisis retrospectivo en el Hospital Nacional Arzoispo Loayza, 2002-2007. Rev peru epidemiol 2009;13(2):3-7.
Nakatani S, Mitsutake K, Ohara T, et al. Recent Picture of Infective Endocarditis in Japan. Circ J 2013;77:1558-64.
Cecchi E, Chirillo F, Castiglione A, et al. Clinical epidemiology in Italian Registry of Infective Endocarditis (RIEI): Focus on age, intravascular devices and enterococci. International Journal of Cardiology 190 (2015):151-6. DOI: http://dx.doi.org/10.1016/j.ijcard.2015.04.123.
Pant S, Patel NJ, Deshmukh A, et al. Trends in infective endocarditis incidence, microbiology, and valve replacement in the United States from 2000 to 2011. J Am Coll Cardiol. 2015;65(19):2070-76.
Stockins B, Neira V, Paredes A, et al. Perfil clínico-epidemiológico de pacientes con endocarditis infecciosa, period 2003-2010 en el hospital de Temuco, Chile. Rev Med Chile 2012; 140:1304-11.
W.G. Fowler, J.M. Miro, B. Hoen, et al., for the ICE Investigators, Staphylococcus aureus endocarditis. A consequence of medical progress, JAMA 293 (2005) 312–21.
S. Leone, V. Ravasio, E. Durante-Mangoni, et al., Epidemiology, characteristics, and outcome of infective endocarditis in Italy: the Italian Study on Endocarditis, Infection 40 (2012) 527–35. DOI: 10.1007/s15010-012-0285-y
Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: The International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med 2009;169:463-73. doi: 10.1001/archinternmed.2008.603.
Vilacosta I, Graupner C, San Román JA, et al. Risk of embolization after institution of antibiotic therapy for infective endocarditis. JAmCollCardiol. 2002;39(9):1489-95. doi:10.1016/s0735-1097(02)01790-4.
Cabell CH, Jollis JG, Peterson GE, et al. Changing patient characteristics and the effect on mortality in endocarditis. Arch Intern Med. 2002; 162(1):90–4. [PubMed: 11784225]
Merello L, Salazar R, Elgueta F et al. Hospital mortality and long-term survival of 103 patients with infective endocarditis requiring surgery. Rev Med Chile 2019; 147:1535-42