Recommendations for the management of ST elevation myocardial infarction after reperfusion
DOI:
https://doi.org/10.47487/apcyccv.v6i3.508Keywords:
Acute Coronary Syndromes, Myocardial Infarction, Heart Failure, Myocardial RevascularizationAbstract
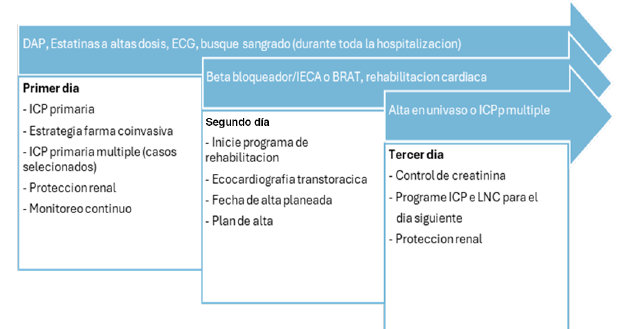
The management of ST-segment elevation acute myocardial infarction after reperfusion involves critical decisions for patients with multivessel disease (MVD), acute heart failure, and left ventricular (LV) thrombus. Complete revascularization of non-culprit lesions ≥70% is recommended during the initial intervention or within the first 19 days, particularly in stable patients. Coronary artery bypass grafting is indicated for high-risk anatomies or complex lesions following a successful coronary intervention, where a hybrid strategy combines percutaneous intervention with surgery, with timing adjusted based on whether a stent was implanted. Post-infarction heart failure is common (28-31%) and requires urgent treatment. Continuous monitoring and prompt intervention can reduce complications. In cases of shock or mechanical complications, an intra-aortic balloon pump and inotropic support may be necessary. Right ventricular infarction is managed with volume support, urgent revascularization, and, if needed, pharmacological support or pacing. LV thrombus, which is more common in previous infarcts with LVEF <50%, requires early diagnosis through echocardiography and/or tomography, along with early anticoagulation, preferably with warfarin, considering triple therapy in cases of high thrombotic risk. This manuscript presents recommendations aimed at optimizing prognosis through early and personalized interventions based on the most recent evidence.
Downloads
References
Park D, Clare R, Schulte P, Pieper K, Shaw L, Califf R, et al. Extension, Location and Clinical Significance of Non-Infarct-Related Coronary Artery Disease among patients with ST-Elevation Myocardial Infarction. JAMA. 2014;312(19):2019-27. doi: 10.1001/jama.2014.15095.
Brieger D, Cullen L, Briffa T, Zaman S, Scott I, Papendick C, et al. National Heart Foundation of Australia & Cardiac Society of Australia and New Zeland: Comprehensive Australian Clinical Guide for Diagnosing and Managing Acute Coronary Syndromes 2025. Heart Lung Circ. 2025;34(4):309-397. doi: 10.1016/j.hlc.2025.02.102.
Rao S, O´Donoghue M, Ruel M, Rab T, Tamis-Holland J, Mukherjee D, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary síndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2025;85(22):2135-2237. doi: 10.1016/j.jacc.2024.11.009.
Stähli B, Varbella F, Schuarz B, Felix S, Seiffert M, Kesterke R, et al. Timing of Complete Revascularization with Multivessel PCI for Myocardial Infarction. N Engl J Med. 2023;389(15):1368-1379. doi: 10.1056/NEJMoa2307823.
Dehghani P, Cantor W, Wang J, Wood D, Storey R, Mehran R, et al. Complete Revascularization in Patients Undergoing a Pharmacoinvasive Strategy for ST-Segment Elevation Myocardial Infarction. Insigts From the COMPLETE Trial. Circ Cardiovasc Interv. 2021;14(8):e010458. doi: 10.1161/CIRCINTERVENTIONS.120.010458.
Figini F, Chen S, Sheiban I. ST-Elevation Myocardial Infarction and Multivessel Coronary Artery Disease – A Critical Review of Current Practice, Evidence and Meta-analyses. Heart International 2020;14(2):80-5. doi: 10.17925/HI.2020.14.2.80.
Fernandez Daza E, Fernandez Juan E, Moreno Mejia I, Moreno Mejía M. Aproximación al diagnóstico de enfermedades hepáticas por el laboratorio clínico. Med Lab. 2008;14(11-12):533-546.
Cataldo Miranda P, Gasevic D, Trin C, Stub D, Zoungas S, Kaye D, et al. Beta-Blocker Therapy After Myocardial Infarction. JACC Adv. 2025;4(3):101582. doi: 10.1016/j.jacadv.2024.101582.
Kaul S. Reevaluating Beta-Blocker Recomendations Post-Myocardial Infarction : Perspective on the 2025 Guideline Update J Am Coll Cardiol. 2025;85(22):2096-9. doi: 10.1016/j.jacc.2025.03.539.
Fontes-Carvalho R, Abreu A, Bento L, Infante de Oliveira E, Pereira H, Freitas J, et al. Post-myocardial infarction patient pathway in Portugal. Rev Port Cardiol. 2025;44(7):457-463. doi 10.1016/j.repc.2024.12.009.
Joint Commission International (JCI). Joint Commission International Accreditation Standards for Hospitals. 8th Edition. JCI; 2024.
Seto A, Shroff A, Abu-Fadel M, Blankenship J, Boudoulas K, Cigarroa J, et al. Length of stay following percutaneous coronary intervention: An expert consensus document update from the society for cardiovascular angiography and interventions. Catheter Cardiovasc Interv. 2018;92(4):717-31. doi: 10.1002/ccd.27637.
Rosselló X, Gonzáles-Del-Hoyo M, Aktaa S, Gale C, Barbash I, Claeys M, et al. European Society of Cardiology quality indicators for the management of acute coronary syndromes: developed in collaboration with the Association for Acute Cardiovascular Care and the European Association of Percutaneous Cardiovascular Interventions of the ESC. Eur Heart J Acute Cardiovasc Care. 2025;14(3):145-154. doi: 10.1093/ehjacc/zuaf014.
Kastrati A, Coughlan J, Ndrepepa G. Primary PCI, Late Presenting STEMI, and the Limits of Time. J Am Coll Cardiol. 2021;78(13):1306-8. doi: 10.1016/j.jacc.2021.08.001.
Chacón-Diaz M, Barrios-Escalante J, Espinoza-Alva D. Registry of “early latecomer” patients with acute ST-segment elevation myocardial infarction at the Instituto Nacional Cardiovascular INCOR – Perú. Arch Cardiol Mex. 2016;86(2):130-9. doi: 10.1016/j.acmx.2015.08.007.
Byrne R, Rosello X, Couglan J, Barbato E, Berry C, Chieffo A, et al. Guía ESC 2023 sobre el diagnóstico y tratamiento de los síndromes coronarios agudos. Madrid: Sociedad Europea de Cardiología (ESC); 2023. doi: 10.1093/eurheartj/ehad191.
Sabaté M. Revascularization of the Infarct-Related Artery. J Am Coll Cardiol. 2008;51(9):965-967. doi: 10.1016/j.jacc.2008.01.003.
Besola L, Colli A, De Caterina R. Coronary bypass surgery for multivessel disease after percutaneous coronary intervention in acute coronary syndromes: why, whom, how early? Eur Heart J. 2024;45(34):3124-3131. doi: 10.1093/eurheartj/ehae413.
Zahrai A, Rahmouni K, Rubens F. Optimal timing of surgical revascularization in patients with acute myocardial infarction. Vessel Plus. 2023;7:32. doi: 10.20517/2574-1209.2023.100.
Silvain J, Abtan J, Kerneis M, Martin R, Finzi J, Vignalou J, et al. Impact of Red Blood Cell Transfusion on Platelet Aggregation and Inflammatory Response in Anemic Coronary and Noncoronary Patients. The TRANSFUSION-2 Study. J Am Coll Cardiol. 2014;63(13):1289-96. doi: 10.1016/j.jacc.2013.11.029.
Chacón-Diaz M, Rodríguez R, Miranda D, Custodio-Sánchez P, Montesinos A, Yábar G, et al. Tratamiento del infarto agudo de miocardio en el Perú y su relación con eventos adversos intrahospitalarios: resultados del segundo registro peruano de infarto de miocardio con elevación del segmento ST (PERSTEMI-II). Arch Peru Cardiol Cir Cardiovasc. 2021;2(2):86-95. 10.47487/apcyccv.v2i2.132.
Pfeffer M, Claggett B, Lewis E, Granger C, Køber L, Maggioni A, et al. Angiotensin Receptor-Neprilysin Inhibition in Acute Myocardial Infarction. N Engl J Med. 2021;385(20):1845-55. doi: 10.1056/ NEJMoa2104508.
Butler J, Jones W, Udell A, Anker S, Petrie M, Harrington J, et al. Empaglifozin after Acute Myocardial Infarction. N Engl J Med. 2024;390(16):1455-66. doi: 10.1056/NEJMoa2314051.
Flaherty J, Bax J, De Luca L, Rossi J, Davinson C, Gheorghiade M, et al. Acute Heart Failure Syndromes for Patients With Coronary Artery Disease. J Am Coll Cardiol. 2009;53(3):254-63. doi: 10.1016/j. jacc.2008.08.072.
Harjola V, Parissis J, Bauersachs J, Brunner-La Rocca H, Bueno H, Ĉelutkienė J, et al. Acute coronary syndromes and acute heart failure: a diagnostic dilemma and high risk combination. A statement from the Acute Heart Failure Committee of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2020;22(8):1298- 1314. doi: 10.1002/ejhf.1831.
Mullens W, Damman K, Harjola C, Mebazaa A, Brunner-La Rocca H, Martens P, et al. The use of diuretics in heart failure with congestion – a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019;21(2):137-155. doi: 10.1002/ejhf.1369.
Ferrero L, Di Cosco O, Grieve S, Bravo L, González M, Nebreda M, et al. Correlación entre la clasificación de Killip-Kimball y la mortalidad de pacientes con IAM, a 55 años de su creación. Rev Fed Arg Cardiol. 2022;51(3):115-119.
Ponce-Gallegos M, Mendoza-Mujica M, Ponce Gallegos J, GarcíaDiaz J, Zelada Pineda J, Araiza- Garaygordobil D, et al. Killip and Kimball classification in the Ultrasound era: Is it time to redefine? Arch Peru Cardiol Cir Cardiovasc. 2024;5(3):153-156. doi: 10.47487/ apcyccv.v5i3.413.
Ducharme A, Zieroth S, Ahooja V, Anderson K, Andrade J, BoivinProulx L, et al. Canadian Cardiovascular Society-Canadian Heart Failure Society Focused Clinical Practice Update of Patients With Differing Heart Failure Phenotypes. Can J Cardiol. 2023;39(8):1030- 1040. doi: 10.1016/j.cjca.2023.04.022.
Falik C, Sobotka P, Dunlap M. Sympathetically Mediated Changes in Capacitance. Circ Heart Fail. 2011;4(5):669-675. doi: 10.1161/ CIRCHEARTFAILURE.111.961789.
Chioncel O, Collins S, Ambrosy A, Gheorghiade M, Filippatos G. Pulmonary Oedema-Therapeutic Targets. Card Fail Rev. 2015;1(1):38- 45. doi: 10.15420/CFR.2015.01.01.38.
Solymosi E, Karstle-Gembardt S, Vadász I, Wang L, Neye N, Adrienne Chupin C, et al. Chloride transport-driven alveolar fluid secretion is a major contributor to cardiogenic lung edema. Proc Natl Acad Sci U S A. 2013;110(25):E2308-16. doi: 10.1073/pnas.1216382110.
Kaestke S, Reich C, Yin N, Habazetti H, Weimann J, Kuebler W. Nitric oxide-dependent inhibition of alveolar fluid clearance in hydrostatic lung edema. Am J Physiol Lung Cell Mol Physiol. 2007;293(4):L859-L969. doi: 10.1152/ajplung.00008.2007.
Cotter G, Moshkovitz Y, Milovanov O, Salah A, Blatt A, Krakover R, et al. Acute heart failure: a novel approach to its pathogenesis and treatment. Eur J Heart Fail. 2002;4(3):227-234. doi: 10.1016/s1388- 9842(02)00017-x.
Biddle L, Yu P. Effect of Furosemide on Hemodynamics and Lung Water in Acute Pulmonary Edema Secondary to Myocardial Infarction. Am J Cardiol. 1979;43(1):86-90. doi: 10.1016/0002- 9149(79)90049-3.
Dikshit K, Vyden J, Forrester J, Chatterjee K, Prakash R, Swan H. Renal and Extrarenal Hemodynamic Effects of Furosemide in Congestive Heart Failure After Acute Myocardial Infarction. N Engl J Med. 1973;288(21):1087-1090. doi: 10.1056/NEJM197305242882102.
Chiancel O, Mebazaa A, Farmakis D, Abdelhamid M, Lund L, Harjola V, et al. Pathophysiology and clinical use of agents with vasodilator properties in acute heart failure. A Scientific statement of the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur J Heart Fail. 2025;27(6):1067-1088. doi: 10.1002/ejhf.3673.
Tamis-Holland J, Abbott J, Al-Azizi K, Barman N, Bortnick A, Cohen M, et al. SCAI Expert Consensus Statement on the Management of Patients With STEMI Referred for Primary PCI. J Soc Cardiovasc Angiogr Interv. 2024;3(11):102294. doi: 10.1016/j.jscai.2024.102294.
Cossette F, Trifan A, Prėvost-Marcotte G, Doolub G, So D, BeaubienSouligny W, et al. Tailored hydration for the prevention of contrastinduced acute kidney injury after coronary angiogram or PCI: A systematic review and metaanalysis. Am Heart J. 2025;282:93-102. doi: 10.1016/j.ahj.2025.01.002.
Bras S, Aharonian V, Mansukhani P, Moore N, Shen A, Jorgensen M, et al. Hemodynamic-guided fluid administration for the prevention of contrastinduced acute kidney injury: the POSEIDON randomized controlled trial. Lancet. 2014;383.1814-23. doi: 10.1016/S0140-6736(14)60689-9.
MacDonald J, Struthers A. What is the Optimal Serum Potassium Level in Cardiovascular Patients? J Am Coll Cardiol. 2004;43(2):155-61. doi: 10.1016/j.jacc.2003.06.021.
Bahit M, Kochar A, Granger C. Post-Myocardial Infarction Heart Failure. JACC Heart Fail. 2018;6(3):179-86. doi: 10.1016/j.jchf.2017.09.015.
Frantz S, Hundertmark M, Schulz-Menger J, Bengel F, Bauersachs J. Left ventricular remodeling post-myocardial infarction: pathophysiology, imaging, and novel therapies. Eur Heart J. 2022;43(27):2549-2561. doi: 10.1093/eurheartj/ehac223.
Carberry J, Marquis-Gravel G, O´Meara E, Dochertyl K. Where Are We With Treatment and Prevention of Heart Failure in Patients PostMyocardial Infarction? JACC Heart Fail. 2024;12(7):1157-1165. doi: 10.1016/j.jchf.2024.04.025.
Saia F, Grigioni F, Marzocchi A, Branzi A. Management of acute left ventricular dysfunction after primary percutaneous coronary intervention for ST elevation acute myocardial infarction. Am Heart J. 2010;160(6 Suppl):S16-21. doi: 10.1016/j.ahj.2010.10.011.
Moiseyev V, Pōder P, Andrejevs N, Ruda M, Golikov A, Lazebnik L, et al. Safety and efficacy of novel calcium sensitizer, levosimendan, in patients with left ventricular failure due to an acute myocardial infarction. RUSSLAN Study. Eur Heart J Fail. 2002;23(18):1422-1432. doi: 10.1053/euhj.2001.3158.
Gillespie T, Ambos H, Sobel E, Roberts R. Effects of Dobutamine in Patients With Acute Myocardial Infarction. Am J Cardiol. 1977;39(4):588-94. doi: 10.1016/s0002-9149(77)80170-7.
Goldstein J. Pathophysiology and Management of Right Heart Ischemia. J Am Coll Cardiol. 2002;40(5):841-53. doi: 10.1016/s0735- 1097(02)02048-x.
Goldstein J, Lerakis S, Moreno P. Right Ventricular Myocardial Infarction-A Tale of Two Ventricles: JACC Focus Seminar 1/5. J Am Coll Cardiol. 2024;83(18):1779-1798. doi: 10.1016/j.jacc.2023.09.839.
Goldstein J, Harada A, Yagi Y, Barzilai B, Cox J. Hemodynamic importance of systolic ventricular interaction, augmented right atrial contractility and atrioventricular synchrony in acute right ventricular dysfunction. J Am Coll Cardiol. 1990;16(1):181-9. doi: 10.1016/0735- 1097(90)90477-7.
Inohara T, Kohsaka S, Fukuda K, Menon V. The challenges in the management of right ventricular infarction. Eur Heart J Acute Cardiovasc Care. 2013;2(3):226-34. doi: 10.1177/2048872613490122.
Love J, Haffagee C, Gore J, Alpert J. Reversibility of hypotension and shock by atrial or atrioventricular sequential pacing in patients with right ventricular infarction. Am Heart J. 1984;108(1):5-13. doi: 10.1016/0002-8703(84)90537-4.
Asinger RW, Mikell F, Elsperger J, Hodges M. Incidence of leftventricular thrombosis after acute transmural myocardial infarction. Serial evaluation by two-dimensional echocardiography. N Engl J Med. 1981;305(6):297-302. doi: 10.1056/NEJM198108063050601.
Pizzetti G, Belotti G, Margonato A, Carlino M, Gerosa S, Carandente O, et al. Thrombolytic therapy reduces the incidence of left ventricular thrombus after anterior myocardial infarction. Relationship to vessel patency and infarct size. Eur Heart J. 1996;17(3):421-8. doi: 10.1093/ oxfordjournals.eurheartj.a014875.
Bulluck H, Chan M, Paradies V, Yellon R, Ho H, Chan MY, et al. Incidence and predictors of left ventricular thrombus by cardiovascular magnetic resonance in acute ST-segment elevation myocardial infarction treated by primary percutaneous coronary intervention: a meta-analysis. J Cardiovasc Magn Reson. 2018;20(1):72. doi: 10.1186/s12968-018-0494-3.
Camaj A, Fuster V, Giustino G, Bienstock SW, Sternheim D, Mehran R, et al. Left Ventricular Thrombus Following Acute Myocardial Infarction: JACC State-of-the-Art Review. J Am Coll Cardiol. 2022;79(10):1010- 1022. doi: 10.1016/j.jacc.2022.01.011.
Di Odoardo L, Bianco M, Gil I, Motolese IG, Chinaglia A, Vicenzi M, et al. Left Ventricular Thrombus Management After Acute Myocardial Infarction in Clinical Practice: Results from LEVITATION Survey and Narrative Review. Cardiovasc Drugs Ther. 2024 Jun;38(3):483-492. doi: 10.1007/s10557-022-07417-w.
Zhang Z, Si D, Zhang Q, Jin L, Heng H, Qu M, et al. Prophylactic Rivaroxaban Therapy for Left Ventricular Thrombus After Anterior ST-Segment Elevation Myocardial Infarction. JACC Cardiovasc Interv. 2022;15(8):861-872. doi: 10.1016/j.jcin.2022.01.285.
Zwart B, Bor WL, de Veer A, Mahmoodi BK, Kelder JC, Lip GYH, et al. A novel risk score to identify the need for triple antithrombotic therapy in patients with atrial fibrillation undergoing percutaneous coronary intervention: a post hoc analysis of the RE-DUAL PCI trial. EuroIntervention. 2022;18(4):e292-e302. doi: 10.4244/ EIJ-D-21-00165.
Levine GN, McEvoy JW, Fang JC, Ibeh C, McCarthy CP, Misra A, et al. American Heart Association Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; and Stroke Council. Management of Patients at Risk for and With Left Ventricular Thrombus: A Scientific Statement From the American Heart Association. Circulation. 2022;146(15):e205-e223. doi: 10.1161/ CIR.0000000000001092.
Bertolin-Boronat C, Marcos-Garcés V, Merenciano-González H, Perez N, Pérez Del Villar C, Gavara J, et al. Prediction of left ventricular thrombus after myocardial infarction: a cardiac magnetic resonance-based prospective registry. Eur J Intern Med. 2025;131:104-112. doi: 10.1016/j.ejim.2024.09.015.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.