Follow-up of patients with myocardial ischemia and non-obstructive coronary lesions
DOI:
https://doi.org/10.47487/apcyccv.v6i2.472Keywords:
Microcirculation, Myocardial Ischemia, Coronary AngiographyAbstract
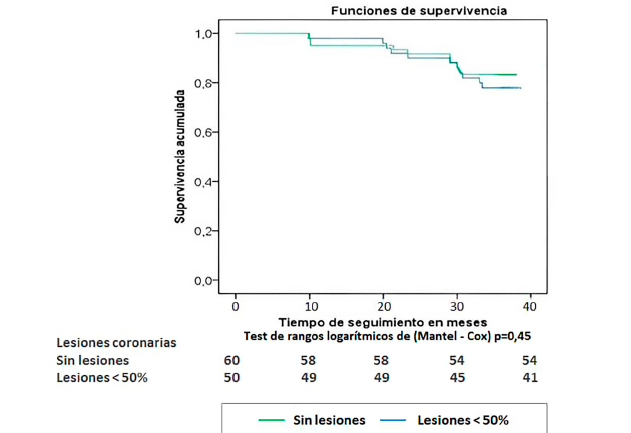
Objective. The presence of coronary lesions of less than 50% in patients with myocardial ischaemia is a common diagnosis in cardiac catheterisation laboratories. The aim of this study was to determine the clinical course of patients with myocardial ischaemia in the absence of obstructive coronary lesions. Materials and methods. A prospective analytical study was conducted in 110 patients of both sexes with documented myocardial ischaemia and coronary lesions of less than 50% on coronary angiography. The follow-up period was three years. Results. The mean age was 64.5 ± 7.2 years, with a predominance of females (57%). The most prevalent risk factors were hypertension (58.2%) and dyslipidaemia (44.5%). In 8.3% of cases, re-hospitalisation was required, with heart failure reported as the leading cause (6.5%). Cardiovascular event-free survival during follow-up was 80%, and was higher in patients without coronary lesions. A higher incidence of cardiovascular events was associated with diabetes mellitus, a family history of ischaemic heart disease, and chronic kidney disease. Conclusions. Patients with myocardial ischaemia in the absence of obstructive coronary lesions experienced adverse events during follow-up, particularly those with diabetes mellitus, a family history of ischaemic heart disease, and chronic kidney disease.
Downloads
References
Organización Mundial de la Salud. Enfermedades cardiovasculares, datos y cifras [Internet]. Ginebra, Suiza: OMS; c2023 [citado el 12 de enero del 2025]. Disponible en: https://www.who.int/es/news-room/ fact-sheets/detail/cardiovascular-diseases-(cvds)
Heusch G. Myocardial ischemia/reperfusion: Translational pathophysiology of ischemic heart disease. Med (N Y) [Internet]. 2024;5(1):10–31. Disponible en: http://dx.doi.org/10.1016/j.medj.2023.12.007
AlShaikh S, Rohm CL, Sutton NR, Burgess SN, Alasnag M. INOCA: Ischemia in non-obstructive coronary arteries. Am Heart J Plus. 2024;42:100391. doi: 10.1016/j.ahjo.2024.100391.
Mehta PK, Huang J, Levit RD, Malas W, Waheed N, Bairey Merz CN. Ischemia and no obstructive coronary arteries (INOCA): A narrative review. Atherosclerosis [Internet]. 2022;363:8–21. Disponible en: http://dx.doi.org/10.1016/j.atherosclerosis.2022.11.009
Chen C, Wei J, AlBadri A, Zarrini P, Bairey Merz CN. Coronary Microvascular Dysfunction - Epidemiology, Pathogenesis, Prognosis, Diagnosis, Risk Factors and Therapy. Circ J. 2016;81(1):3-11. doi: 10.1253/circj.CJ-16-1002.
Hansen B, Holtzman JN, Juszczynski C, Khan N, Kaur G, Varma B, et al. Ischemia with no obstructive arteries (INOCA): A review of the prevalence, diagnosis and management. Curr Probl Cardiol. 2023;48(1):101420. doi: 10.1016/j.cpcardiol.2022.101420.
Hasdai D, Gibbons RJ, Holmes DR Jr, Higano ST, Lerman A. Coronary endothelial dysfunction in humans is associated with myocardial perfusion defects. Circulation. 1997;96(10):3390-5. doi: 10.1161/01.cir.96.10.3390.
Frobert O, Molgaard H, Botker HE, Bagger JP. Autonomic balance in patients with angina and a normal coronary angiogram. Eur Heart J. 1995;16(10):1356-60. doi: 10.1093/oxfordjournals.eurheartj.a060742.
Jespersen L, Hvelplund A, Abildstrøm SZ, Pedersen F, Galatius S, Madsen JK, et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J. 2012;33(6):734-44. doi: 10.1093/ eurheartj/ehr331.
Patel MR, Chen AY, Peterson ED, Newby LK, Pollack CV Jr, Brindis RG, et al. Prevalence, predictors, and outcomes of patients with non-ST-segment elevation myocardial infarction and insignificant coronary artery disease: Results from the Can Rapid risk stratification of Unstable angina patients Suppress Adverse outcomes with Early implementation of the ACC/AHA Guidelines (CRUSADE) initiative. Am Heart J. 2006;152(4):641-7. doi: 10.1016/j.ahj.2006.02.035.
Min JK, Dunning A, Lin FY, Achenbach S, Al-Mallah M, Budoff MJ, et al. Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol. 2011;58(8):849-60. doi: 10.1016/j.jacc.2011.02.074.
Izquierdo Coronel B, Lopez País J, Galan Gil D, Espinosa Pascual MJ, Awamleh P, Martínez Peredo CG, et al. Myocardial infarction with non-obstructive coronary arteries (MINOCA) according to definitions of 2016 ESC position paper, perfil clinic. J American Col Cardiol. 2018;71(11_Supplement):A19.
Patel KK, Spertus JA, Chan PS, Sperry BW, Thompson RC, Al Badarin F, et al. Extent of myocardial ischemia on positron emission tomography and survival benefit with early revascularization. J Am Coll Cardiol. 2019;74(13):1645-1654. doi: 10.1016/j.jacc.2019.07.055.
Jespersen L, Abildstrom SZ, Hvelplund A, Madsen JK, Galatius S, Pedersen F, et al. Burden and Hospital Admission and repeat angiography in angina pectoris patients with and without coronary artery disease: a registry based cohort study. PLoS One. 2014;9(4):e93170. doi: 10.1371/journal.pone.0093170.
Sharaf B, Wood T, Shaw L, Johnson BD, Kelsey S, Anderson RD, et al. Adverse outcomes among women presenting with signs and symptoms of ischemia and no obstructive coronary artery disease: findings from the National Heart, Lung, and Blood Institute-sponsored Women’s Ischemia Syndrome Evaluation (WISE) angiographic core laboratory. Am Heart J. 2013;166(1):134-41. doi: 10.1016/j.ahj.2013.04.002.
Konst RE, Meeder JG, Wittekoek ME, Maas AHEM, Appelman Y, Piek JJ, et al. Ischemia with no obstructive coronary arteries. Neth Heart J. 2020;28(Suppl 1):66-72. doi: 10.1007/s12471-020-01451-9.
Shimokawa H, Suda A, Takahashi J, Berry C, Camici PG, Crea F, et al. Clinical characteristics and prognosis of patients with microvascular angina: an international and prospective cohort study by the Coronary Vasomotor Disorders International Study (COVADIS) Group. Eur Heart J. 2021;42(44):4592-4600. doi: 10.1093/eurheartj/ehab282.
Pacheco Claudio C, Quesada O, Pepine CJ, Noel Bairey Merz C. Why names matter for women: MINOCA/INOCA (myocardial infarction/ ischemia and no obstructive coronary artery disease). Clin Cardiol. 2018;41(2):185-193. doi: 10.1002/clc.22894.
Maddox TM, Stanislawski MA, Grunwald GK, Bradley SM, Ho PM, Tsai TT, et al. Nonobstructive coronary artery disease and risk of myocardial infarction. JAMA. 2014;312(17):1754-63. doi: 10.1001/jama.2014.14681.
Schumann CL, Mathew RC, Dean JL, Yang Y, Balfour PC Jr, Shaw PW, et al. Functional and Economic Impact of INOCA and Influence of Coronary Microvascular Dysfunction. JACC Cardiovasc Imaging. 2021;14(7):1369-1379. doi: 10.1016/j.jcmg.2021.01.041.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














