Pharmacological treatment of patients with chronic heart failure: a subanalysis of an ecuadorian registry
DOI:
https://doi.org/10.47487/apcyccv.v6i2.470Keywords:
Heart Failure, Treatment, PrognosisAbstract
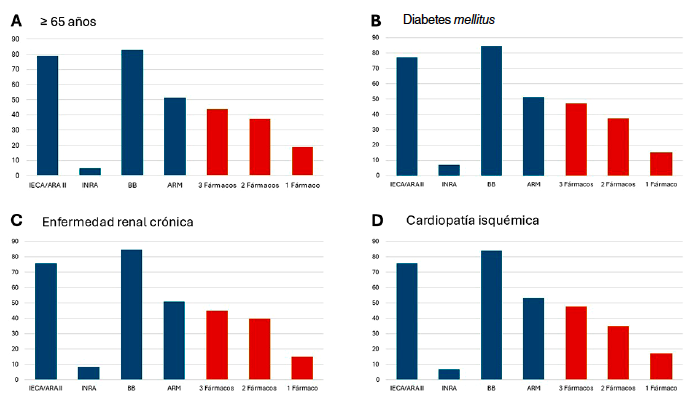
Introduction. Introduction. In Ecuador, there is limited data on the treatment of patients with heart failure (HF). Objective. This study aimed to determine the rate of use of prognosis-modifying drugs and their association with prognosis. Materials and methods. A retrospective observational study was conducted on patients with chronic HF included in the “Los Ceibos” registry between January 2017 and December 2022. Patients were followed for a median of 2.28 years (interquartile range [IQR]: 1.25-3.49). Results. A total of 711 patients diagnosed with HF were included. Among them, 82.7% (n=588) received angiotensin-converting enzyme inhibitors (ACEIs), angiotensin receptor blockers (ARBs), or angiotensin receptor–neprilysin inhibitors (ARNIs); 82.3% (n=585) received beta-blockers (BBs); and 51.3% (n=365) were treated with mineralocorticoid receptor antagonists (MRAs). Among patients with HFrEF, those receiving triple therapy (ACEI/ARB/ARNI + BB + MRA) had lower all-cause mortality compared to other groups (38.8%, log-rank p=0.014). In patients with Heart Failure with preserved Ejection Fraction (HFpEF), no mortality differences were observed according to the number of medications used (log-rank p=0.720). MRA use was not associated with a prognostic benefit in HFpEF (p>0.05). Patients receiving triple therapy with ARNI + BB + MRA had better survival during follow-up compared to any other drug combination (log-rank p=0.027). Conclusions. A high rate of ACEI/ARB/ARNI and BB use was observed. The use of triple therapy, particularly the combination of ARNI + BB + MRA, was associated with improved prognosis in patients with HFrEF over a four-year follow-up period. No prognostic benefit of MRA use was observed in patients with HFpEF.
Downloads
References
Moreno-Rondón L, Ortega-Armas ME, Coronel A, Vaca I, Guevara B, Alarcón Cedeño R, et al. Characteristics, treatment and prognosis of patients with chronic heart failure according to ejection fraction. Results of an Ecuadorian registry. Acta Cardiol. 2024;79(8):942-952. doi: 10.1080/00015385.2024.2392335.
Yan T, Zhu S, Yin X, Xie C, Xue J, Zhu M, et al. Burden, Trends, and Inequalities of Heart Failure Globally, 1990 to 2019: A Secondary Analysis Based on the Global Burden of Disease 2019 Study. J Am Heart Assoc. 2023;12(6):e027852. doi:10.1161/JAHA.122.027852
Hessel FP. Overview of the socio-economic consequences of heart failure. Cardiovasc Diagn Ther. 2021 Feb;11(1):254-262. doi: 10.21037/ cdt-20-291.
Cook C, Cole G, Asaria P, Jabbour R, Francis DP. The annual global economic burden of heart failure. Int J Cardiol. 2014;171(3):368-376. doi:10.1016/j.ijcard.2013.12.028
Brahmbhatt DH, Rayner DG, Foroutan F. If Heart Failure Medications Provide So Much Benefit, Why Do So Few Patients Receive Them? JACC Heart Fail. 2022;10(5):367. doi:10.1016/j.jchf.2022.02.014
Greene SJ, Butler J, Albert NM, DeVore AD, Sharma PP, Duffy CI, et al. Medical Therapy for Heart Failure With Reduced Ejection Fraction: The CHAMP-HF Registry. J Am Coll Cardiol. 2018;72(4):351-366. doi:10.1016/j.jacc.2018.04.070
Wirtz HS, Sheer R, Honarpour N, Casebeer AW, Simmons JD, Kurtz CE, et al. Real‐World Analysis of Guideline‐Based Therapy After Hospitalization for Heart Failure. J Am Heart Assoc. 2020;9(16):e015042. doi: 10.1161/JAHA.119.015042.
Tromp J, Ouwerkerk W, van Veldhuisen DJ, Hillege HL, Richards AM, van der Meer P, et al. A Systematic Review and Network Meta-Analysis of Pharmacological Treatment of Heart Failure With Reduced Ejection Fraction. JACC Heart Fail. 2022;10(2):73-84. doi:10.1016/j.jchf.2021.09.004.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2023;44(37):3627-3639. doi:10.1093/eurheartj/ehad195.
Kittleson MM, Panjrath GS, Amancherla K, Davis LL, Deswal A, Dixon DL, et al. 2023 ACC Expert Consensus Decision Pathway on Management of Heart Failure With Preserved Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2023;81(18):1835-1878. doi: 10.1016/j.jacc.2023.03.393.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(17):1757-1780. doi:10.1016/j.jacc.2021.12.011.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599-3726. doi:10.1093/eurheartj/ehab368.
Straw S, McGinlay M, Witte KK. Four pillars of heart failure: contemporary pharmacological therapy for heart failure with reduced ejection fraction. Open Heart. 2021;8(1):e001585. doi:10.1136/openhrt-2021-001585.
Gomez-Mesa JE, Saldarriaga C, Echeverría LE, Rivera-Toquica A, Luna P, Campbell S, et al. Characteristics and Outcomes of Heart Failure Patients from a Middle-Income Country: The RECOLFACA Registry. Glob Heart. 2022;17(1):57. doi:10.5334/gh.1145.
Crespo-Leiro MG, Anker SD, Maggioni AP, Coats AJ, Filippatos G, Ruschitzka F, et al. European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur J Heart Fail. 2016;18(6):613-625. doi:10.1002/ejhf.566.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. Guía ESC 2016 sobre el diagnóstico y tratamiento de la insuficiencia cardiaca aguda y crónica. Rev Esp Cardiol. 2016;69(12):1167.e1-1167. e85. doi:10.1016/j.recesp.2016.10.014.
Packer M, Anker SD, Butler J, Filippatos G, Ferreira JP, Pocock SJ, et al. Influence of neprilysin inhibition on the efficacy and safety of empagliflozin in patients with chronic heart failure and a reduced ejection fraction: the EMPEROR-Reduced trial. Eur Heart J. 2021;42(6):671-680. doi:10.1093/eurheartj/ehaa968.
Solomon SD, Jhund PS, Claggett BL, Dewan P, Køber L, Kosiborod MN, et al. Effect of Dapagliflozin in Patients With HFrEF Treated With Sacubitril/Valsartan: The DAPA-HF Trial. JACC Heart Fail. 2020;8(10):811-818. doi:10.1016/j.jchf.2020.04.008.
Senni M, Alemayehu WG, Sim D, Edelmann F, Butler J, Ezekowitz J, et al. Efficacy and safety of vericiguat in patients with heart failure with reduced ejection fraction treated with sacubitril/valsartan: insights from the VICTORIA trial. Eur J Heart Fail. 2022;24(9):1614- 1622. doi:10.1002/ejhf.2608.
Mann DL, Givertz MM, Vader JM, Starling RC, Shah P, McNulty SE, et al. Effect of Treatment With Sacubitril/Valsartan in Patients With Advanced Heart Failure and Reduced Ejection Fraction: A Randomized Clinical Trial. JAMA Cardiology. 2022;7(1):17-25. doi:10.1001/jamacardio.2021.4567.
De Marzo V, Savarese G, Tricarico L, Hassan S, Iacoviello M, Porto I, et al. Network meta-analysis of medical therapy efficacy in more than 90,000 patients with heart failure and reduced ejection fraction. J Intern Med. 2022;292(2):333-349. doi:10.1111/joim.13487.
Savarese G, Kishi T, Vardeny O, Adamsson Eryd S, Bodegård J, Lund LH, et al. Heart Failure Drug Treatment—Inertia, Titration, and Discontinuation. JACC: Heart Failure. 2023;11(1):1-14. doi:10.1016/j. jchf.2022.08.009.
Meifang W, Ying W, Wen C, Kaizu X, Meiyan S, Liming L. Advance in the pharmacological and comorbidities management of heart failure with preserved ejection fraction: evidence from clinical trials. Heart Fail Rev. 2024;29(2):305-320. doi:10.1007/s10741-023-10338-x.
Giannopoulos G, Kousta M, Anagnostopoulos I, Karageorgiou S, Myrovali E, Deftereos G, et al. Advances in Heart Failure with Preserved Ejection Fraction Management - The Role of SacubitrilValsartan, Pirfenidone, Spironolactone and Empagliflozin: Is Success a Series of Small Victories? Curr Pharm Des. 2023;29(7):502-508. doi: 10.2174/1381612829666230202141437.
Liu F, Chen Y, Feng X, Teng Z, Yuan Y, Bin J. Effects of beta-blockers on heart failure with preserved ejection fraction: a meta-analysis. PLoS One. 2014;9(3):e90555. doi:10.1371/journal.pone.0090555.
Lund LH, Benson L, Dahlström U, Edner M, Friberg L. Association between use of β-blockers and outcomes in patients with heart failure and preserved ejection fraction. JAMA. 2014;312(19):2008- 2018. doi:10.1001/jama.2014.15241.
Meyer M, Du Fay Lavallaz J, Benson L, Savarese G, Dahlström U, Lund LH. Association Between β-Blockers and Outcomes in Heart Failure With Preserved Ejection Fraction: Current Insights From the SwedeHF Registry. J Card Fail. 2021;27(11):1165-1174. doi:10.1016/j. cardfail.2021.04.015.
Kittleson MM, Panjrath GS, Amancherla K, Davis LL, Deswal A, Dixon DL, et al. 2023 ACC Expert Consensus Decision Pathway on Management of Heart Failure With Preserved Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2023;81(18):1835-1878. doi:10.1016/j. jacc.2023.03.393.
Solomon SD, McMurray JJV, Vaduganathan M, Claggett B, Jhund PS, Desai AS, et al. Finerenone in Heart Failure with Mildly Reduced or Preserved Ejection Fraction. N Engl J Med. 2024;391(16):1475-1485. doi:10.1056/NEJMoa2407107.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














