Detrimental impact of acute coronary syndrome on theindependence of the elderly
DOI:
https://doi.org/10.47487/apcyccv.v6i1.454Keywords:
Acute Coronary Syndrome, Functional Status, ElderlyAbstract
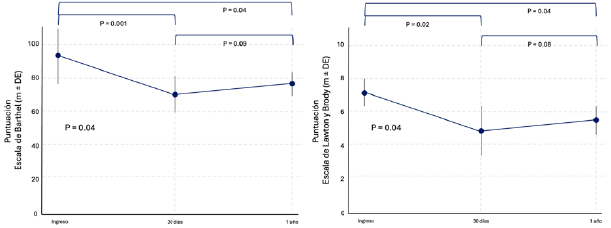
Objectives. To evaluate the prognostic role of functional status in older adults hospitalized for acute coronary syndrome (ACS) and the implications of the coronary event on functional decline during follow-up. Materials and methods. This was a single-center, prospective cohort study including patients aged ≥65 years hospitalized for ACS with (STEMI) or without ST-segment elevation in 2022. Patients with total dependence or lacking a care network were excluded. Functional status was assessed using the Barthel Index and the Lawton and Brody scales at admission, 30 days, and one year post-discharge. The association between initial functional status and major adverse cardiovascular events (MACE) was analyzed, as well as the impact of ACS on functional status over the short and long term. Results. A total of 110 patients older than 65 years were included (mean age 78.8±4.6 years; 61.8% male). At admission, 94.3% presented mild functional dependence according to the Barthel Index, with similar findings on the Lawton and Brody scales. At 30 days, a significant functional decline was observed (Barthel: 71.2±11.3, p<0.001; Lawton: 4.8±2.5, p=0.02), which persisted at one year. Initial functional status was not associated with MACE. ST-segment elevation ACS (STEMI) was an independent predictor of short-term functional decline (adjusted OR 1.75; p=0.04). Conclusions. In older adults with ACS, initial functional status did not predict adverse events; however, significant functional decline was observed, particularly after STEMI. This underscores the importance of personalized strategies for managing this vulnerable population.
Downloads
References
Timmis A, Kazakiewicz D, Townsend N, Huculeci R, Aboyans V, Vardas P. Global epidemiology of acute coronary syndromes. Nat Rev Cardiol. 2023;20(11):778-88. doi: 10.1038/s41569-023-00884-0.
D’imperio H, Charask A, Costa YC, Zapata G, Quiroga M, Meiriño A, et al. Acute Myocardial Infarction in Argentina. Third ARGEN-IAM-ST Registry Report and 8-Year Mortality Behavior. Rev Argent Cardiol. 2023;91(6):435-42.
Briggs R, McDonough A, Ellis G, Bennett K, O’Neill D, Robinson D. Comprehensive Geriatric Assessment for community-dwelling, high-risk, frail, older people. Cochrane Database Syst Rev. 2022;5(5):CD012705. doi: 10.1002/14651858.CD012705.pub2.
Rozzini R, Bianchetti A, Alboni P, Baldasseroni S, Bo M, Boccanelli A, et al. The older patient with cardiovascular disease: background and clinical implications of the comprehensive geriatric assessment. Minerva Med. 2022;113(4):609-15. doi: 10.23736/S0026-4806.22.08086-7.
Damluji AA, Huang J, Bandeen-Roche K, Forman DE, Gerstenblith G, Moscucci M, et al. Frailty Among Older Adults With Acute Myocardial Infarction and Outcomes From Percutaneous Coronary Interventions. J Am Heart Assoc. 2019;8(17):e013686. doi: 10.1161/JAHA.119.013686.
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138(20):e618-51. doi: 10.1161/CIR.0000000000000617.
Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. Percutaneous Coronary Intervention versus Coronary-Artery Bypass Grafting for Severe Coronary Artery Disease. N Engl J Med. 2009;360(10):961-72. doi: 10.1056/NEJMoa0804626.
Gibson CM, Cannon CP, Daley WL, Dodge JT, Alexander B, Marble SJ, et al. TIMI frame count: A quantitative method of assessing coronary artery flow. Circulation. 1996;93(5):879-88. doi: 10.1161/01.cir.93.5.879.
Mehran R, Rao S V., Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736-47. doi: 10.1161/CIRCULATIONAHA.110.009449.
Mahoney Fi, Barthel Dw. Functional evaluation: the barthel index. Md State Med J. 1965;14:61-5.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179-86.
Consenso de Infarto Agudo de Miocardio con Elevación del Segmento ST Actualización focalizada. 2020 [Internet]. Caba: Sociedad Argentina de Cardiología; c2024 [citado el 28 de diciembre de 2024]. Disponible en: https://www.sac.org.ar/sac-consensos/consenso-de-infarto-agudo-de-miocardio-con-elevacion-delsegmento-st-actualizacion-focalizada-2020/
Consenso de Síndromes Coronarios Agudos Sin elevación del Segmento ST-2020 [Internet]. Caba: Sociedad Argentina de Cardiología; c2024 [citado el 28 de diciembre de 2024]. Disponible en: https://www.sac.org.ar/sac-consensos/consenso-de-sindromescoronarios-agudos-sin-elevacion-del-segmento-st-2020/
Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44(38):3720-826. doi: 10.1093/eurheartj/ehad191.
Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/ SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;144(22):E368-454. doi: 10.1161/CIR.0000000000001029.
Gibbon B. Measuring stroke recovery. Nurs Times. 1991;87(44):32-4. 17. Mao HF, Chang LH, Tsai AYJ, Huang WNW, Tang LY, Lee HJ, et al. Diagnostic accuracy of Instrumental Activities of Daily Living for dementia in community-dwelling older adults. Age Ageing. 2018;47(4):551-7. doi: 10.1093/ageing/afy021.
Jabłonowska-Babij P, Olszewska-Szopa M, Potoczek S, Majcherek M, Szeremet A, Kujawa K, et al. The Role of the Lawton Instrumental Activities of Daily Living (IADL) Scale in Predicting Adverse Events and Outcomes of R-CHOP Treatment in Elderly Patients with Diffuse Large B-Cell Lymphomas (DLBCLs) or Mantle Cell Lymphomas (MCLs): A Prospective Single-Center Study. Cancers (Basel). 2024;16(24):4170. doi: 10.3390/cancers16244170.
Sanchis J, Bonanad C, García-Blas S, Ruiz V, Fernández-Cisnal A, Sastre C, et al. Long-Term Prognostic Value of Cognitive Impairment on Top of Frailty in Older Adults after Acute Coronary Syndrome. J Clin Med. 2021;10(3):444. doi: 10.3390/jcm10030444.
Wontor R, Lisiak M, Łoboz-Rudnicka M, Ołpińska B, Wyderka R, Dudek K, et al. The Impact of the Coexistence of Frailty Syndrome and Cognitive Impairment on Early and Midterm Complications in Older Patients with Acute Coronary Syndromes. J Clin Med. 2024;13(23):7408. doi: 10.3390/jcm13237408.
Formiga F, Chivite D, Solé A, Manito N, Ramon JM, Pujol R. Functional outcomes of elderly patients after the first hospital admission for decompensated heart failure (HF). A prospective study. Arch Gerontol Geriatr. 2006;43(2):175-85. doi: 10.1016/j.archger.2005.10.010.
Gordo F, Castro C, Torrejón I, Bartolomé S, Coca F, Abella A. [Functional status as an independent risk factor in elderly patients admitted to an Intensive Care Unit]. Rev Esp Geriatr Gerontol. 2018;53(4):213-6. doi: 10.1016/j.regg.2017.08.002.
Calvo E, Formiga F, Andreu-Periz L, Ariza-Solé A, Gómez-Hospital JA, Comín-Colet J. [Components of geriatric assessment and therapeutic adherence in elderly patients with acute myocardial infarction]. Rev Esp Geriatr Gerontol. 2022;57(1):28-32. doi: 10.1016/j.regg.2021.06.002.
Alfaraidhy MA, Regan C, Forman DE. Cardiac rehabilitation for older adults: current evidence and future potential. Expert Rev Cardiovasc Ther. 2022;20(1):13-34. doi: 10.1080/14779072.2022.2035722.
Menezes AR, Lavie CJ, Forman DE, Arena R, Milani R V, Franklin BA. Cardiac rehabilitation in the elderly. Prog Cardiovasc Dis. 2014;57(2):152-9. doi: 10.1016/j.pcad.2014.01.002.
Ma L, Zhu X, Tang Y, Li X, Dong Q, Xu J, et al. Best Evidence Summary for Cardiac Exercise Rehabilitation after PCI in Patients with Acute Myocardial Infarction [Internet]. [cited 2025 Jan 3]. Disponible en: https://kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&filename=SYXL202103002&dbname=CJFDAUTO
Munir H, Fromowitz J, Goldfarb M. Early mobilization post-myocardial infarction: A scoping review. PLoS One. 2020;15(8):e0237866. doi: 10.1371/journal.pone.0237866.
Mejía PJC, Cassano PD, Morón PD, Reátegui MD, Navarrete KM, Córdova-Mendoza P. Prevalence of anxiety and depression in patients with acute coronary syndrome: systematic review and meta-analysis. Pan Afr Med J. 2023;46:91. doi: 10.11604/pamj.2023.46.91.41792.
Mouhat B, Putot A, Hanon O, Eicher JC, Chagué F, Beer JC, et al. Low systolic blood pressure and mortality in elderly patients after acute myocardial infarction. J Am Heart Assoc. 2020;9(5):e013030. doi: 10.1161/JAHA.119.013030.
Johnston S, Eckhardt AL. Fatigue and acute coronary syndrome: a systematic review of contributing factors. Heart Lung. 2018;47(3):192-204. doi: 10.1016/j.hrtlng.2018.03.005.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














