Trends in the epidemiology of acute myocardial infarction in Peru: An analysis of the official SUSALUD records
DOI:
https://doi.org/10.47487/apcyccv.v5i4.435Keywords:
Cardiovascular Diseases, Myocardial Infarction, Epidemiology, PeruAbstract
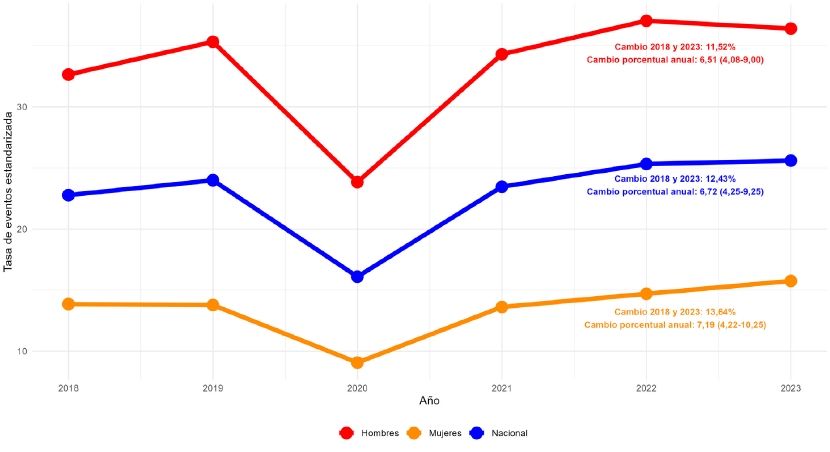
Objective. To determine the age-standardized rate of acute myocardial infarction (AMI) events and its trend in recent years. Materials and methods. An ecological study of secondary data on morbidity in emergency areas of Peruvian hospitals between 2018 and 2023 was conducted. Cases of AMI in adults aged 20 years or older were identified using ICD-10 codes. Age-standardized AMI event rates per 100,000 person-years were calculated. In addition, the change in event rate between extreme years was calculated, and a Poisson regression was used to estimate the annual percentage change in event rates along with their 95% confidence interval (CI), adjusting for age and calendar year. These rates were stratified by sex and political-administrative regions. Results. 28,088 AMI events were recorded between 2018 and 2023. The national age-standardized rate increased from 22.77 in 2018 to 25.60 per 100,000 person-years in 2023, with an annual percentage change of 6.72% (95% CI 4.25-9.25). Men had higher AMI event rates compared to women throughout the study period. In addition, the highest event rates were observed in the Constitutional Province of Callao, San Martin and Loreto. Conclusions. Our findings provide a better understanding of the epidemiology of AMI in Peru and its evolution in recent years, important data to improve prevention, treatment and resource distribution strategies for the management of AMI.
Downloads
References
World Heart Federation. World Heart Report 2023: Confronting the World’s Number One Killer [Internet]. Geneva, Switzerland: World Heart Federation; 2023 [citado el 9 de octubre de 2024]. Disponible en: https://world-heart-federation.org/wp-content/uploads/World-Heart-Report-2023.pdf
Salari N, Morddarvanjoghi F, Abdolmaleki A, Rasoulpoor S, Khaleghi AA, Hezarkhani LA, et al. The global prevalence of myocardial infarction: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2023;23(1):206. doi: 10.1186/s12872-023-03231-w.
Camacho X, Nedkoff L, Wright FL, Nghiem N, Buajitti E, Goldacre R, et al. Relative contribution of trends in myocardial infarction event rates and case fatality to declines in mortality: an international comparative study of 1·95 million events in 80·4 million people in four countries. Lancet Public Health. 2022;7(3):e229-39.
Reynolds K, Go AS, Leong TK, Boudreau DM, Cassidy-Bushrow AE, Fortmann SP, et al. Trends in Incidence of Hospitalized Acute Myocardial Infarction in the Cardiovascular Research Network (CVRN). Am J Med. 2017;130(3):317-27. doi: 10.1016/j.amjmed.2016.09.014.
Timmis A, Vardas P, Townsend N, Torbica A, Katus H, De Smedt D, et al. European Society of Cardiology: cardiovascular disease statistics 2021. Eur Heart J. 2022;43(8):716-99. doi: 10.1093/eurheartj/ehab892.
Chang J, Deng Q, Guo M, Ezzati M, Baumgartner J, Bixby H, et al. Trends and Inequalities in the Incidence of Acute Myocardial Infarction among Beijing Townships, 2007–2018. Int J Environ Res Public Health. 2021;18(23):12276. doi: 10.3390/ijerph182312276.
Seo Y, Moon J, Lee HH, Kim HC, Kaneko F, Shin S, et al. Incidence and case fatality of acute myocardial infarction in Korea, 2011-2020. Epidemiol Health. 2024;46:e2024002. doi: 10.4178/epih.e2024002.
Nazzal C, Lefian A, Alonso F. Incidencia de infarto agudo de miocardio en Chile, 2008-2016. Rev Médica Chile. 2021;149(3):323-9. doi: 10.4067/s0034-98872021000300323.
World Health Organization. ICD-10 : international statistical classification of diseases and related health problems : tenth revision [Internet]. 2nd ed. Geneva: World Health Organization; 2004 [citado el 9 de octubre de 2024]. Disponible en: https://iris.who.int/handle/10665/42980
Aragon TJ, Fay MP, Wollschlaeger D, Omidpanah A. Package ‘epitools’ [Internet]. Citeseer; 2017 [citado el 10 de octubre de 2024]. Disponible en: https://cran.r-project.org/web/packages/epitools/epitools.pdf
Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age standardization of rates: a new WHO standard [Internet]. GPE Discussion Paper Series: No.31. Geneva: World Health Organization; 2001 [citado el 10 de octubre de 2024]. Disponible en: https://cdn.who.int/media/docs/default-source/gho-documents/global-health-zestimates/gpe_discussion_paper_series_paper31_2001_age_standardization_rates.pdf
Stent-Save a Life Initiative Project. Stent-Save a Life! - Reducing mortality from acute coronary syndromes [Internet]. Stent-Save a Life! 2024 [citado el 10 de octubre de 2024]. Disponible en: https://www.stentsavealife.com/
Kumar R, Ammar A, Qayyum D, Mujtaba M, Siddiqui MN, Khan MQ, et al. Increasing Incidence of ST-Elevation Acute Coronary Syndrome in Young South Asian Population, a Challenge for the World? An Assessment of Clinical and Angiographic Patterns and Hospital Course of Premature Acute Myocardial Infarction. Am J Cardiol. 2023;205:190-197. doi: 10.1016/j.amjcard.2023.07.138.
Lanas F, Avezum A, Bautista LE, Diaz R, Luna M, Islam S, et al. Risk Factors for Acute Myocardial Infarction in Latin America: The INTERHEART Latin American Study. Circulation. 2007;115(9):1067-74. doi: 10.1161/CIRCULATIONAHA.106.633552.
Steyn K, Sliwa K, Hawken S, Commerford P, Onen C, Damasceno A, et al. Risk Factors Associated With Myocardial Infarction in Africa: The INTERHEART Africa Study. Circulation. 2005;112(23):3554-61. doi: 10.1161/CIRCULATIONAHA.105.563452.
Naghavi M, Ong KL, Aali A, Ababneh HS, Abate YH, Abbafati C, et al. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2100-2132. doi: 10.1016/S0140-6736(24)00367-2.
Chacón-Diaz M, Rodríguez Olivares R, Miranda-Noé D, Custodio-Sánchez P, Montesinos Cárdenas A, Yabar Galindo G, et al. Tratamiento del infarto agudo de miocardio en el Perú y su relación con eventos adversos intrahospitalarios: resultados del Segundo Registro Peruano de Infarto de Miocardio con elevación del segmento ST (PERSTEMI-II). Arch Peru Cardiol Cir Cardiovasc. 2021;2(2):86-95. doi: 10.47487/apcyccv.v2i2.132.
Chacón-Diaz M, Hernández Vásquez A, Custodio-Sánchez P. Sobrevida al año en pacientes con infarto de miocardio con elevación del segmento ST en el Perú. Arch Peru Cardiol Cir Cardiovasc. 2022;3(2):53-9. doi: 10.47487/apcyccv.v3i2.218.
United Nations. Goal 3 Ensure healthy lives and promote well-being for all at all ages [Internet]. 2024 [citado el 11 de octubre de 2024]. Disponible en: https://sdgs.un.org/goals/goal3#targets_and_indicators
Kinoshita K, Ozato N, Yamaguchi T, Bushita H, Sudo M, Yamashiro Y, et al. Association of the COVID-19 pandemic with changes in objectively measured sedentary behaviour and adiposity. Int J Obes (Lond). 2023;47(5):375-381. doi: 10.1038/s41366-023-01274-9.
Zhang T, Mei Q, Zhang Z, Walline JH, Liu Y, Zhu H, et al. Risk for newly diagnosed diabetes after COVID-19: a systematic review and meta-analysis. BMC Med. 2022;20(1):444. doi: 10.1186/s12916-022-02656-y. 22. Nour TY, Altintaş KH. Effect of the COVID-19 pandemic on obesity and its risk factors: a systematic review. BMC Public Health. 2023;23(1):1018. doi: 10.1186/s12889-023-15833-2.
Silva DRPD, Werneck AO, Malta DC, Souza Júnior PRBD, Azevedo LO, Barros MBDA, et al. Changes in the prevalence of physical inactivity and sedentary behavior during COVID-19 pandemic: a survey with 39,693 Brazilian adults. Cad Saude Publica. 2021;37(3):e00221920. doi: 10.1590/0102-311X00221920.
Nadarajah R, Wu J, Hurdus B, Asma S, Bhatt DL, Biondi-Zoccai G, et al. The collateral damage of COVID-19 to cardiovascular services: a meta-analysis. Eur Heart J. 2022;43(33):3164-3178. doi: 10.1093/eurheartj/ehac227.
Mayol J, Artucio C, Batista I, Puentes A, Villegas J, Quizpe R, et al. An international survey in Latin America on the practice of interventional cardiology during the COVID-19 pandemic, with a particular focus on myocardial infarction. Neth Heart J. 2020;28(7-8):424-430. doi: 10.1007/s12471-020-01440-y.
Fornasini M, Sisa I, Baldeon ME. Increased Cardiovascular Mortality in Ecuador during COVID-19 Pandemic. Ann Glob Health. 2023;89(1):21. doi: 10.5334/aogh.4021.
Carrión Arcela JP, Custodio-Sánchez P, Coca Caycho TG. Impacto de la pandemia COVID-19 en el abordaje del infarto de miocardio con elevación del segmento ST en un centro de referencia del norte del Perú. Arch Peru Cardiol Cir Cardiovasc. 2021;2(3):159-66. doi: 10.47487/apcyccv.v2i3.148.
Soto A. Barreras para una atención eficaz en los hospitales de referencia del Ministerio de Salud del Perú: atendiendo pacientes en el siglo XXI con recursos del siglo XX. Rev Peru Med Exp Salud Pública. 2019;36(2):304-311. doi: 10.17843/rpmesp.2019.362.4425.
Albrektsen G, Heuch I, Løchen ML, Thelle DS, Wilsgaard T, Njølstad I, et al. Lifelong Gender Gap in Risk of Incident Myocardial Infarction: The Tromsø Study. JAMA Intern Med. 2016;176(11):1673-1679. doi: 10.1001/jamainternmed.2016.5451.
Crea F, Battipaglia I, Andreotti F. Sex differences in mechanisms, presentation and management of ischaemic heart disease. Atherosclerosis. 2015;241(1):157-68. doi: 10.1016/j.atherosclerosis.2015.04.802.
Hage FG, Oparil S. Ovarian hormones and vascular disease. Curr Opin Cardiol. 2013;28(4):411-6. doi: 10.1097/HCO.0b013e32836205e7.
Collet JP, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42(14):1289-367. doi: 10.1093/eurheartj/ehaa575.
Centers for Disease Control and Prevention. Classification of Diseases, Functioning, and Disability. Atlanta: CDC; 2024 [citado el 10 de octubre de 2024]. Disponible en: https://www.cdc.gov/nchs/icd/icd-10-cm/index.html
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40(3):237-69. doi: 10.1093/eurheartj/ehy462.
McCarthy CP, Kolte D, Kennedy KF, Pandey A, Raber I, Oseran A, et al. Hospitalizations and Outcomes of T1MI Observed Before and After the Introduction of MI Subtype Codes. J Am Coll Cardiol. 2021;78(12):1242-1253. doi: 10.1016/j.jacc.2021.07.034.
Carrillo-Larco RM, Guzman-Vilca WC, Leon-Velarde F, Bernabe-Ortiz A, Jimenez MM, Penny ME, et al. Peru – Progress in health and sciences in 200 years of independence. Lancet Reg Health Am. 2021;7:100148. doi: 10.1016/j.lana.2021.100148.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














