Analysis of cardiac surgeries and operative mortality at the National Cardiovascular Institute during 2022
DOI:
https://doi.org/10.47487/apcyccv.v4i2.287Keywords:
Cardiac Surgical Procedures, Clinical Evolution, PeruAbstract
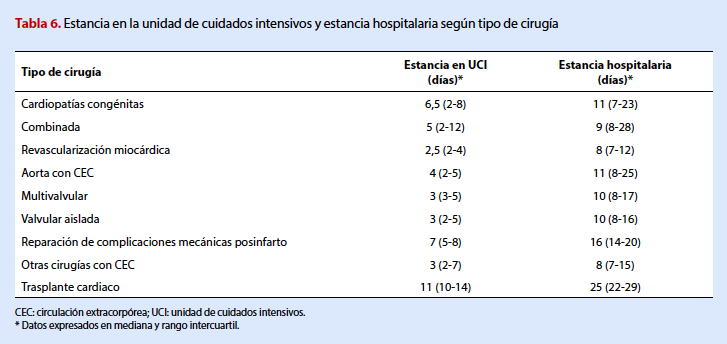
Objective. To describe cardiac surgeries, their approaches, and determine operative mortality according to the type of surgery and the main complications recorded within 30 days postoperatively, performed at the National Cardiovascular Institute of Peru. Materials and methods. A descriptive study was conducted on all patients over 18 years of age who underwent cardiovascular surgery at the National Cardiovascular Institute “Carlos Alberto Peschiera Carrillo”. Results. During the year 2022, a total of 503 cardiac surgeries were performed. Of the patients undergoing surgery, 63.6% (320) were males. Isolated valvular surgery, primarily aortic or mitral valve replacement, was the most frequent surgical procedure, with 136 surgeries (27.0%). This was followed by myocardial revascularization surgery with 110 procedures (21.9%). Throughout the year, there were 23 deaths, resulting in an overall mortality rate of 4.5%. The mortality rate for elective surgeries was 2.8%, while for emergency surgeries, it was 14.3%. The most common complication was paroxysmal atrial fibrillation (14.0%), followed by surgical site infection with 52 cases (10.3%). Conclusions. Valvular surgery, whether isolated or combined with other procedures, was the most frequently performed. The obtained mortality rate is considered acceptable for a reference center.
Downloads
References
World Health Organization. Global Status Report on Noncommunicable Diseases 2010. Geneva; 2011 [citado 10 de abril de 2023]. Disponible en: https://apps.who.int/iris/bitstream/ handle/10665/44579/9789240686458_eng.pdf.
Global Cardiac Surgery [Internet]. Global Cardiac Surgery. 2018 [citado 10 de abril de 2023]. Disponible en: https://globalcardiacsurgery.com/ global-cardiac-surgery/
Vervoort D, Meuris B, Meyns B, Verbrugghe P. Global cardiac surgery: Access to cardiac surgical care around the world. J Thorac Cardiovasc Surg. 2020;159(3):987-996.e6. doi: 10.1016/j.jtcvs.2019.04.039.
Chávarry-Infante P, Ríos-Ortega JC, Gonzáles-Castro S, Salas- Escobedo G, Abanto-Guiop F, Salas-Lor M. Experiencia inicial en el tratamiento del síndrome aórtico agudo en un hospital del Ministerio de Salud del Perú. Venciendo las adversidades. Cir Cardiov. 2023. https://doi.org/10.1016/j.circv.2023.05.001.
Sánchez-Moreno F. El sistema nacional de salud en el Perú. Rev Peru Med Exp Salud Publica. 2014;31(4):747-53.
Lowenstein D, Guardiani F, Pieroni P, et al. Realidad de la cirugía cardiaca en la República Argentina: Registro CONAREC XVI. Rev Argent Cardiol. 2010;78(3):228-237.
Rodríguez-Hernández A, García-Torres M, Bucio Reta E, Baranda-Tovar FM. Análisis de mortalidad y estancia hospitalaria en cirugía cardiaca en México 2015: datos del Instituto Nacional de Cardiología. Arch Cardiol Mex. 2018;88(5):397-402. doi: 10.1016/j.acmx.2017.11.004.
Salamanca MA, Cuba E, Castillo-De la Cadena L, Vidal D, Salamanca MA, Cuba E, et al. Características de las intervenciones en cirugía cardiaca en un hospital general de Lima, Perú. Rev Med Hered. 2022;33(4):227-236.
Cuerpo Caballero G, Carnero Alcázar M, López Menéndez J, Centella Hernández T, Polo López L, García Fuster R, et al. Cirugía cardiovascular en España en el año 2020. Registro de intervenciones de la Sociedad Española de Cirugía Cardiovascular y Endovascular. Cir Cardiov. 2022;29(4):207–20. doi: 10.1016/j.circv.2022.03.023.
Kim KM, Arghami A, Habib R, Daneshmand MA, Parsons N, Elhalabi Z, et al. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2022 Update on Outcomes and Research. Ann Thorac Surg. 2023;115(3):566-574. doi: 10.1016/j.athoracsur.2022.12.033.
Gomes WJ, Moreira RS, Zilli AC, Bettiati Jr LC, Figueira FAM dos S, D’Azevedo SSP, et al. The Brazilian Registry of Adult Patient Undergoing Cardiovascular Surgery, the BYPASS Project: Results of the First 1,722 Patients. Braz J Cardiovasc Surg. 2017;32(2):71-76. doi: 10.21470/1678-9741-2017-0053.
GP-G, HAS-T. Supervisión: JR-O, VR-V, GP-G. Redacción – borrador original: GP-G, FWM-N, HAS-T. Redacción – revisión y edición: JR-O, VR-V, GP-G, FWM-N, HAS-T.
Gaudino M, Rahouma M, Abouarab A, Leonard J, Kamel M, Di Franco A, et al. Radial artery versus saphenous vein as the second conduit for coronary artery bypass surgery: A meta-analysis. J Thorac Cardiovasc Surg. 2019;157(5):1819-1825.e10. doi: 10.1016/j.jtcvs.2018.08.123.
Qureshi SH, Boulemden A, Darwin O, Shanmuganathan S, Szafranek A, Naik S. Multiarterial coronary grafting using the radial artery as a second arterial graft: how far does the survival benefit extend? Eur J Cardiothorac Surg. 2021;61(1):216-224. doi: 10.1093/ejcts/ezab308.
Gaudino M, Benedetto U, Fremes S, Biondi-Zoccai G, Sedrakyan A, Puskas JD, et al. Radial-Artery or Saphenous-Vein Grafts in Coronary- Artery Bypass Surgery. N Engl J Med. 2018;378(22):2069-2077. doi: 10.1056/NEJMoa1716026.
Bowdish ME, D’Agostino RS, Thourani VH, Schwann TA, Krohn C, Desai N, et al. STS Adult Cardiac Surgery Database: 2021 Update on Outcomes, Quality, and Research. Ann Thorac Surg. 2021;111(6):1770- 1780. doi: 10.1016/j.athoracsur.2021.03.043.
D’Agostino RS, Jacobs JP, Badhwar V, Paone G, Rankin JS, Han JM, et al. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2017 Update on Outcomes and Quality. Ann Thorac Surg. 2017;103(1):18-24. doi: 10.1016/j.athoracsur.2016.11.001.
Mitrev Z, Anguseva T. Emergencies in cardiovascular surgery. J Cardiothorac Surg. 2013;8(Suppl 1):O2. doi: 10.1186/1749-8090- 8-S1-O2.
D’Agostino RS, Jacobs JP, Badhwar V, Fernandez FG, Paone G, Wormuth DW, et al. The Society of Thoracic Surgeons Adult Cardiac Surgery Database: 2018 Update on Outcomes and Quality. Ann Thorac Surg. 2018;105(1):15-23. doi: 10.1016/j.athoracsur.2017.10.035.
Pahwa S, Bernabei A, Schaff H, Stulak J, Greason K, Pochettino A, et al. Impact of postoperative complications after cardiac surgery on long- term survival. J Card Surg. 2021;36(6):2045-2052. doi: 10.1111/jocs.15471.
Schumer EM, Chaney JH, Trivedi JR, Linsky PL, Williams ML, Slaughter MS. Emergency Coronary Artery Bypass Grafting: Indications and Outcomes from 2003 through 2013. Tex Heart Inst J. 2016;43(3):214-9. doi: 10.14503/THIJ-14-4978.
Oliveira EL de, Westphal GA, Mastroeni MF. Demographic and clinical characteristics of patients undergoing coronary artery bypass graft surgery and their relation to mortality. Rev Bras Cir Cardiovasc. 2012;27(1):52-60. doi: 10.5935/1678-9741.20120009.
Siregar S, Groenwold RH, Versteegh MI, Takkenberg JJ, Bots ML, Van Der Graaf Y, et al. Data Resource Profile: adult cardiac surgery database of the Netherlands Association for Cardio-Thoracic Surgery. Int J Epidemiol. 2013;42(1):142-9. doi: 10.1093/ije/dys241.
Downloads
Published
Issue
Section
License
Copyright (c) 2023 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














