The adult with tetralogy of Fallot: what the clinical cardiologist needs to know
DOI:
https://doi.org/10.47487/apcyccv.v2i2.138Keywords:
Tetralogy of Fallot, Survival, Adults, Heart failureAbstract
Tetralogy of Fallot (TOF) is the most common cyanotic congenital heart disease. After more than seven decades of the first palliative surgery, TOF prognosis has changed dramatically. With a higher survival into adulthood, the clinical cardiologist faces challenges in the management of this population, from severe pulmonary regurgitation to heart failure and ventricular arrhythmias. In this review, we will describe the most relevant aspects of the care of adults with this disease.
Downloads
References
Diaz-Frias J, Guillaume M. Tetralogy of Fallot. StatPearls. Treasure Island (FL), 2021.
Taussig HB. Neuhauser Lecture: Tetralogy of Fallot: early history and late results. AJR American journal of roentgenology 1979;133:422-31.
Babu-Narayan S, Gatzoulis MA. Tetralogy of Fallot. In: Diagnosis and Management of Adult Congenital Heart Disease. 3rd Edition. ElSevier. 2018.
Pérez-Lescure Picarzo J, Mosquera González M, Latasa Zamalloa P, Crespo Marcos D. Incidence and evolution of congenital heart disease in Spain from 2003 until 2012. An Pediatr. 2018 Nov 1;89(5):294–301. Disponible en: https://www.analesdepediatria.org/es-incidencia-evolucion-cardiopatias-congenitas-espana-articulo-S1695403318300043.
Pinto Junior VC, Branco KM, Cavalcante RC, et al. Epidemiology of congenital heart disease in Brazil. Revista brasileira de cirurgia cardiovascular : orgao oficial da Sociedade Brasileira de Cirurgia Cardiovascular. 2015;30:219-24.
Benavides-Lara A, Faerron Angel JE, Umana Solis L, Romero Zuniga JJ. [Epidemiology and registry of congenital heart disease in Costa Rica]. Revista panamericana de salud publica = Pan American journal of public health 2011;30:31-8.
Tassinari S, Martínez-Vernaza S, Erazo-Morera N, Pinzón-Arciniegas MC, Gracia G, Zarante I. Epidemiología de las cardiopatías congénitas en Bogotá, Colombia en el período comprendido entre 2001 y 2014: ¿Mejoría en la vigilancia o aumento en la prevalencia?. Biomedica. 1 de mayo de 2018;38(Sup1):141-8. Disponible en: https://revistabiomedica.org/index.php/biomedica/article/view/3381.
Martin GR, Ewer AK, Gaviglio A et al. Updated Strategies for Pulse Oximetry Screening for Critical Congenital Heart Disease. Pediatrics 2020;146.
Ayasta Monge AL. Asociación entre altura y cardiopatías congénitas en pacientes pediátricos en el Instituto Nacional de Salud del Niño (INSN), Lima-Perú, en los años 2017-2018. Lima; 2018. Disponible en: http://hdl.handle.net/10757/624870.
Uribe Chávez J, Ramal Asayag C, Olórtegui A, Pisconte C, Elgegren J, Fritas R, et al. Incidencia de cardiopatías congénitas en Iquitos, Perú. Rev Peru Cardiol. 2010;36(1):14–20. Disponible en: http://repebis.upch.edu.pe/articulos/rpc/v36n1/a3.pdf.
Uribe Rivera AK, Díaz-Vélez C, Cerrón-Rivera C. Características epidemiológicas y clínicas de las cardiopatías congénitas en menores de 5 años del Hospital Almanzor Aguinaga Asenjo: Enero - Diciembre 2012. Horiz Med (Barcelona). 2015;15(1):49–56. Disponible en: http://www.scielo.org.pe/scielo.php?pid=S1727-558X2015000100007&script=sci_abstract.
Mandalenakis Z, Giang KW, Eriksson P, et al. Survival in Children With Congenital Heart Disease: Have We Reached a Peak at 97%? Journal of the American Heart Association 2020;9:e017704.
Moons P, Bovijn L, Budts W, Belmans A, Gewillig M. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation 2010;122:2264-72.
Torres-Romucho CE, Uriondo-Ore VG, Ramirez-Palomino AJ, et al. [Factors associated with survival at one year of life in neonates with severe congenital cardiopathy in A National Hospital in Peru]. Revista peruana de medicina experimental y salud publica 2019;36:433-441.
Villafane J, Feinstein JA, Jenkins KJ, et al. Hot topics in tetralogy of Fallot. Journal of the American College of Cardiology 2013;62:2155-66.
Oliveira PHA, Souza BS, Pacheco EN, et al. Genetic Syndromes Associated with Congenital Cardiac Defects and Ophthalmologic Changes - Systematization for Diagnosis in the Clinical Practice. Arquivos brasileiros de cardiologia 2018;110:84-90.
Morgenthau A, Frishman WH. Genetic Origins of Tetralogy of Fallot. Cardiology in review 2018;26:86-92.
Glaeser C, Kotzot D, Caliebe A, et al. Gene symbol: JAG1. Disease: tetralogy of Fallot. Human genetics 2006;119:674.
Rauch R, Hofbeck M, Zweier C, et al. Comprehensive genotype-phenotype analysis in 230 patients with tetralogy of Fallot. Journal of medical genetics 2010;47:321-31.
Mahle WT, Crisalli J, Coleman K, et al. Deletion of chromosome 22q11.2 and outcome in patients with pulmonary atresia and ventricular septal defect. The Annals of thoracic surgery 2003;76:567-71.
Bailliard F, Anderson RH. Tetralogy of Fallot. Orphanet journal of rare diseases 2009;4:2.
Brickner ME, Hillis LD, Lange RA. Congenital heart disease in adults. Second of two parts. The New England journal of medicine 2000;342:334-42.
Wise-Faberowski L, Asija R, McElhinney DB. Tetralogy of Fallot: Everything you wanted to know but were afraid to ask. Paediatric anaesthesia 2019;29:475-482.
Leonard H, Derrick G, O'Sullivan J, Wren C. Natural and unnatural history of pulmonary atresia. Heart 2000;84:499-503.
Bhatt AB, Foster E, Kuehl K, et al. Congenital heart disease in the older adult: a scientific statement from the American Heart Association. Circulation 2015;131:1884-931.
Babu-Narayan SV, Diller GP, Gheta RR, et al. Clinical outcomes of surgical pulmonary valve replacement after repair of tetralogy of Fallot and potential prognostic value of preoperative cardiopulmonary exercise testing. Circulation 2014;129:18-27.
Huehnergarth KV, Gurvitz M, Stout KK, Otto CM. Repaired tetralogy of Fallot in the adult: monitoring and management. Heart 2008;94:1663-9.
Shinebourne EA, Babu-Narayan SV, Carvalho JS. Tetralogy of Fallot: from fetus to adult. Heart 2006;92:1353-9.
Garson A, Jr., Gillette PC, McNamara DG. Propranolol: the preferred palliation for tetralogy of Fallot. The American journal of cardiology 1981;47:1098-104.
Barazzone C, Jaccard C, Berner M, et al. Propranolol treatment in children with tetralogy of Fallot alters the response to isoprenaline after surgical repair. British heart journal 1988;60:156-61.
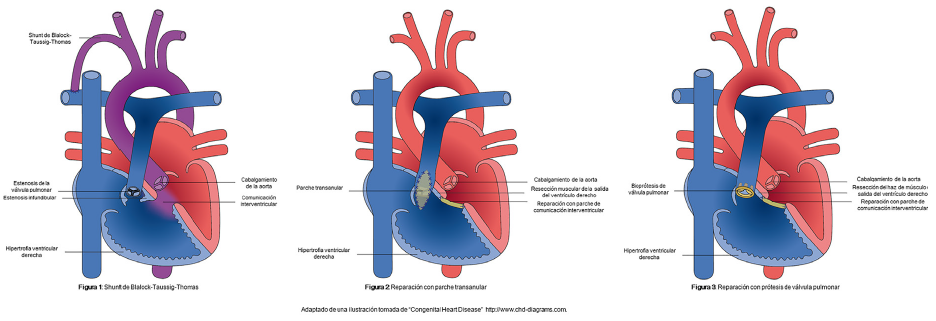
de Leval MR, McKay R, Jones M, Stark J, Macartney FJ. Modified Blalock-Taussig shunt. Use of subclavian artery orifice as flow regulator in prosthetic systemic-pulmonary artery shunts. The Journal of thoracic and cardiovascular surgery 1981;81:112-9.
Rehman R, Marhisham MC, Alwi M. Stenting the complex patent ductus arteriosus in tetralogy of Fallot with pulmonary atresia: challenges and outcomes. Future cardiology 2018;14:55-73.
Sandoval JP, Chaturvedi RR, Benson L, et al. Right Ventricular Outflow Tract Stenting in Tetralogy of Fallot Infants With Risk Factors for Early Primary Repair. Circulation Cardiovascular interventions 2016;9.
Apitz C, Webb GD, Redington AN. Tetralogy of Fallot. Lancet 2009;374:1462-71.
Van Arsdell GS, Maharaj GS, Tom J, et al. What is the optimal age for repair of tetralogy of Fallot? Circulation 2000;102:III123-9.
Mainwaring RD, Hanley FL. Tetralogy of Fallot Repair: How I Teach It. The Annals of thoracic surgery 2016;102:1776-1781.
Geva T, Sandweiss BM, Gauvreau K, Lock JE, Powell AJ. Factors associated with impaired clinical status in long-term survivors of tetralogy of Fallot repair evaluated by magnetic resonance imaging. Journal of the American College of Cardiology 2004;43:1068-74.
Bouzas B, Kilner PJ, Gatzoulis MA. Pulmonary regurgitation: not a benign lesion. European heart journal 2005;26:433-9.
Nollert G, Fischlein T, Bouterwek S, Bohmer C, Klinner W, Reichart B. Long-term survival in patients with repair of tetralogy of Fallot: 36-year follow-up of 490 survivors of the first year after surgical repair. Journal of the American College of Cardiology 1997;30:1374-83.
Bacha EA, Scheule AM, Zurakowski D, et al. Long-term results after early primary repair of tetralogy of Fallot. The Journal of thoracic and cardiovascular surgery 2001;122:154-61.
Krieger EV, Valente AM. Tetralogy of Fallot. Cardiology clinics 2020;38:365-377.
Stout KK, Daniels CJ, Aboulhosn JA, et al. 2018 AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology 2019;73:e81-e192.
Aboulhosn JA, Hijazi ZM. Transcatheter Interventions in Adult Congenital Heart Disease. Cardiology clinics 2020;38:403-416.
Grotenhuis HB, Dallaire F, Verpalen IM, van den Akker MJE, Mertens L, Friedberg MK. Aortic Root Dilatation and Aortic-Related Complications in Children After Tetralogy of Fallot Repair. Circulation Cardiovascular imaging 2018;11:e007611.
Sim HT, Kim JW, Kim SH, Park SJ, Jang SI, Lee CH. Correlation Between Total Repair Timing and Late Aortic Root Dilatation in Repaired Tetralogy of Fallot. Pediatric cardiology 2020;41:1501-1508.
Egbe AC, Crestanello J, Miranda WR, Connolly HM. Thoracic Aortic Dissection in Tetralogy of Fallot: A Review of the National Inpatient Sample Database. Journal of the American Heart Association 2019;8:e011943.
Chang MC, Wu MT, Weng KP, et al. Left ventricular regional myocardial motion and twist function in repaired tetralogy of Fallot evaluated by magnetic resonance tissue phase mapping. European radiology 2018;28:104-114.
Valente AM, Geva T. How to Image Repaired Tetralogy of Fallot. Circulation Cardiovascular imaging 2017;10.
Bokma JP, Winter MM, Oosterhof T, et al. Preoperative thresholds for mid-to-late haemodynamic and clinical outcomes after pulmonary valve replacement in tetralogy of Fallot. European heart journal 2016;37:829-35.
Mouws E, Roos-Hesselink JW, Bogers A, de Groot NMS. Coexistence of tachyarrhythmias in patients with tetralogy of Fallot. Heart rhythm 2018;15:503-511.
Maury P, Sacher F, Rollin A, et al. Ventricular arrhythmias and sudden death in tetralogy of Fallot. Archives of cardiovascular diseases 2017;110:354-362.
Stout KK, Broberg CS, Book WM, et al. Chronic Heart Failure in Congenital Heart Disease: A Scientific Statement From the American Heart Association. Circulation 2016;133:770-801.
Bokma JP, Winter MM, van Dijk AP, et al. Effect of Losartan on Right Ventricular Dysfunction: Results From the Double-Blind, Randomized REDEFINE Trial (Right Ventricular Dysfunction in Tetralogy of Fallot: Inhibition of the Renin-Angiotensin-Aldosterone System) in Adults With Repaired Tetralogy of Fallot. Circulation 2018;137:1463-1471.
Santens B, Van De Bruaene A, De Meester P, et al. Diagnosis and treatment of right ventricular dysfunction in congenital heart disease. Cardiovascular diagnosis and therapy 2020;10:1625-1645.
Menachem JN. Advanced Heart Failure in the ACHD Population: Finding the Fellows' Role in a Growing Field. Journal of the American College of Cardiology 2017;69:1986-1989.
Egbe AC, Kothapalli S, Borlaug BA, et al. Mechanism and Risk Factors for Death in Adults With Tetralogy of Fallot. The American journal of cardiology 2019;124:803-807.
Egbe AC, Miranda WR, Mehra N, et al. Role of QRS Fragmentation for Risk Stratification in Adults With Tetralogy of Fallot. Journal of the American Heart Association 2018;7:e010274.
Bokma JP, Winter MM, Vehmeijer JT, et al. QRS fragmentation is superior to QRS duration in predicting mortality in adults with tetralogy of Fallot. Heart 2017;103:666-671.
Khairy P, Harris L, Landzberg MJ, et al. Implantable cardioverter-defibrillators in tetralogy of Fallot. Circulation 2008;117:363-70.
Wernovsky G, Rome JJ, Tabbutt S, et al. Guidelines for the outpatient management of complex congenital heart disease. Congenital heart disease 2006;1:10-26.
Schwerzmann M, Goossens E, Gallego P, et al. Recommendations for advance care planning in adults with congenital heart disease: a position paper from the ESC Working Group of Adult Congenital Heart Disease, the Association of Cardiovascular Nursing and Allied Professions (ACNAP), the European Association for Palliative Care (EAPC), and the International Society for Adult Congenital Heart Disease (ISACHD). European heart journal 2020;41:4200-4210.
Steiner JM, Dhami A, Brown CE, et al. Barriers and Facilitators of Palliative Care and Advance Care Planning in Adults With Congenital Heart Disease. The American journal of cardiology 2020;135:128-134.