Cardiopatía coronaria isquémica y tuberculosis: una sindemia inadvertida.Revisión de la literatura y propuesta de manejo
DOI:
https://doi.org/10.47487/apcyccv.v5i2.375Palabras clave:
Tuberculosis, Insuficiencia Cardiaca, Enfermedad Coronaria, Infarto del MiocardioResumen
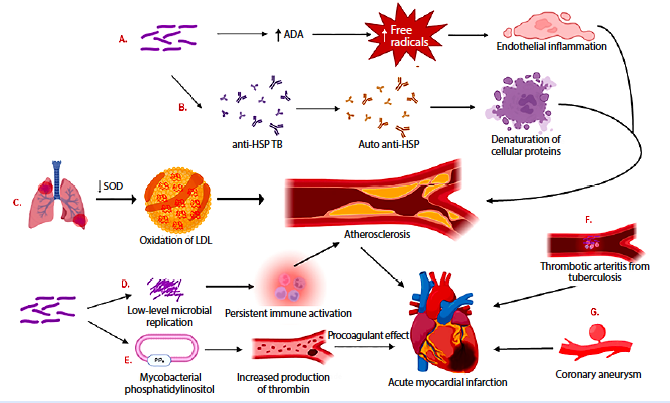
La tuberculosis es una enfermedad que viene en aumento y que afecta cerca de un tercio de la población mundial. En consonancia con el aumento de la tuberculosis, la enfermedad cardiovascular ha tenido un comportamiento similar, de este grupo, la cardiopatía coronaria isquémica se ha convertido en la principal causa de muerte en todo el mundo. Se podría extraer, en base a la literatura, una relación entre la tuberculosis y la cardiopatía coronaria isquémica a través de que comparten múltiples factores de riesgo en común y desde un posible sustrato fisiopatológico que las vincula. La forma conjunta de presentación de estas dos entidades reportada hasta el momento es variada: se ha encontrado como debut de un síndrome coronario agudo en pacientes con tuberculosis activa, el desarrollo progresivo de aterosclerosis coronaria en pacientes con tuberculosis latente, entre otras. Dado este posible vínculo y el aumento progresivo de sus tasas de incidencia podemos afirmar que estamos ante una sindemia inadvertida, siendo su manejo conjunto un desafío por las grandes interacciones farmacológicas. El propósito de esta revisión es esclarecer este posible vínculo, plantear un enfoque para el diagnóstico así como suministrar un algoritmo de tratamiento de todo el espectro de la enfermedad coronaria que coexiste con la tuberculosis de acuerdo con la literatura actual disponible.
Descargas
Referencias
Khan MK, Islam MN, Ferdous J, Alam MM. An Overview on Epidemiology of Tuberculosis. Mymensingh Med J MMJ. 2019;28(1):259-66.
López-López JP, Posada-Martínez EL, Saldarriaga C, Wyss F, Ponte-Negretti CI, Alexander B, et al. Tuberculosis and the heart. J Am Heart Assoc. 2021;10(7). doi: 10.1161/jaha.120.019435.
Natarajan A, Beena PM, Devnikar AV, Mali S. A systemic review on tuberculosis. Indian J Tuberc. 2020;67(3):295-311. doi: 10.1016/j.ijtb.2020.02.005.
Instituto Nacional de Salud. Informe de Evento [Internet]. Bogotá: INS; 2024 [citado 20 de marzo de 2023]. Disponible en: https://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx
Situación epidemiológica de la tuberculosis en el Perú, 2018-2022. Boletin Epidemiológico del Perú [Internet]. 2023;12(20): [citado 28 de marzo de 2024] Disponible en: https://www.dge.gob.pe/epipublic/uploads/boletin/boletin_202320_28_163316.pdf
Djaharuddin I, Amir M, Qanitha A. Exploring the link between cardiovascular risk factors and manifestations in latent tuberculosis infection: a comprehensive literature review. Egypt Heart J.2023;75(1):43.
Ministerio de Salud de Colombia. Enfermedades cardiovasculares [Internet]. Bogotá: Ministerio de Salud; c2024 [citado 20 de marzo de 2023]. Disponible en: https://www.minsalud.gov.co/salud/publica/PENT/Paginas/enfermedades-cardiovasculares.aspx
Enfermedad cardiovascular. Principal causa de muerte en Colombia. Boletin ONS [Internet]. 2013;1 [citado 20 de marzo de 2023]. Disponible en: https://www.ins.gov.co/Direcciones/ONS/Boletines/boletin_web_ONS/boletin1.html
Wang TK, Wong CF, Au WK, Cheng VC, Wong SS. Mycobacterium tuberculosis sternal wound infection after open heart surgery: a case report and review of the literature. Diagn Microbiol Infect Dis. 2007;58(2):245-9. doi: 10.1016/j.diagmicrobio.2006.11.021.
Tabaja H, Hajar Z, Kanj SS. A review of eleven cases of tuberculosis presenting as sternal wound abscess after open heart surgery. Infect Dis Lond Engl. 2017;49(10):721-7. doi: 10.1080/23744235.2017.1347817.
Kälvegren H, Fridfeldt J, Bengtsson T. The role of plasma adenosine deaminase in chemoattractant-stimulated oxygen radical production in neutrophils. Eur J Cell Biol. 2010;89(6):462-7. doi: 10.1016/j.ejcb.2009.12.004.
Huaman M, Qualls J, Jose S, Jose S, Schmidt S, Mousa A, et al. Mycobacterium bovis Bacille-Calmette-Guérin Infection Aggravates Atherosclerosis. Front Immunol. 2020;11:607957. doi: 10.3389/fimmu.2020.607957.
World Health Organization. TB disease burden [Internet]. Geneva: WHO; 2022 [citado el 2 de junio de 2024]. Disponible en: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022/tb-disease-burden
Van Eeden S, Leipsic J, Paul Man SF, Sin DD. The relationship between lung inflammation and cardiovascular disease. Am J Respir Crit Care Med. 2012;186(1):11-6. doi: 10.1164/rccm.201203-0455PP.
Khan Y, Shah M, Shahabuddin S. Incidental finding of tuberculous pleural effusion in patient undergoing coronary artery bypass grafting: Case report. Ann Med Surg. 2019;45:110-2. doi: 10.1016/j.amsu.2019.08.001.
Yuan SM. Sternal wound tuberculosis following cardiac operations: a review. Rev Bras Cir Cardiovasc Órgão Of Soc Bras Cir Cardiovasc. 2015;30(4):489-93. doi: 10.5935/1678-9741.20140102.
Tuladhar SM, Noursadeghi M, Boyle JJ, Friedland JS, Hornick P. Tuberculous pericardial effusion after coronary artery bypass graft. Ann Thorac Surg. 2006;82(4):1519-21. doi: 10.1016/j. athoracsur.2006.02.059.
Wang TK, Wong CF, Au WK, Cheng VC, Wong SS. Mycobacterium tuberculosis sternal wound infection after open heart surgery: a case report and review of the literature. Diagn Microbiol Infect Dis. 2007;58(2):245-9. doi: 10.1016/j.diagmicrobio.2006.11.021.
Ng CSH, Arifi AA, Wan S, Lee TW, Yim APC. Cardiac operation with associated pulmonary resection: a word of caution. Asian Cardiovasc Thorac Ann. 2002;10(4):362-4. doi: 10.1177/021849230201000423.
Bakalli A, Osmani B, Kamberi L, Pllana E. Acute myocardial infarction and pulmonary tuberculosis in a young female patient: a case report. Cases J. 2008;1:246. doi: 10.1186/1757-1626-1-246.
Chan S. An unusual case of mycobacterium tuberculous coronary arteritis and thrombosis resulting in acute myocardial infarction. Forensic Sci Med Pathol. 2018;14(3):390-4. doi: 10.1007/s12024-018-0002-y.
Peddle L, Otto M. Coronary artery tuberculosis: An unusual case of sudden death. Leg Med Tokyo Jpn. 2018;30:56-8. doi: 10.1016/j.legalmed.2017.11.008.
Khalil MW, Grech ED, Al-Mohammed A, Cooper GJ, Sarkar PK. Rapid development of fatal TB constrictive pericarditis after cardiac surgery. J Card Surg. 2006;21(4):417-8. doi: 10.1111/j.1540-8191.2006.00259.x.
Huaman MA, Ticona E, Miranda G, Kryscio RJ, Mugruza R, Aranda E, et al. The Relationship Between Latent Tuberculosis Infection and Acute Myocardial Infarction. Clin Infect Dis Off Publ Infect Dis Soc Am. 2018;66(6):886-92. doi: 10.1093/cid/cix910.
Barreto-Neto N, Segre AW, Guedes LKN, Seguro LPC, Pereira RMR. Resolution of coronary arteritis following tuberculosis treatment. J Clin Tuberc Mycobact Dis. 2022;26:100295. doi: 10.1016/j.jctube.2021.100295
Baluku JB, Nabwana M, Nalunjogi J, Muttamba W, Mubangizi I, Nakiyingi L, et al. Cardiovascular risk factors among people with drug-resistant tuberculosis in Uganda. BMC Cardiovascular Disorders. 2022;22(1):464. doi: 10.1186/s12872-022-02889-y.
Adhikary D, Barman S, Ranjan R, Stone H. A Systematic Review of Major Cardiovascular Risk Factors: A Growing Global Health Concern. Cureus. 2022;14(10):e30119. doi: 10.7759/cureus.30119.
Basham CA, Smith SJ, Romanowski K, Johnston JC. Cardiovascular morbidity and mortality among persons diagnosed with tuberculosis: A systematic review and meta-analysis. PLoS One. 2020;15(7):e0235821. doi: 10.1371/journal.pone.0235821.
Rota S, Rota S. Mycobacterium tuberculosis complex in atherosclerosis. Acta Med Okayama. 2005;59(6):247-51. doi: 10.18926/AMO/31958.
Nezami N, Ghorbanihaghjo A, Rashtchizadeh N, Argani H, Tafrishinejad A, Ghorashi S, et al. Atherogenic changes of low-density lipoprotein susceptibility to oxidation, and antioxidant enzymes in pulmonary tuberculosis. Atherosclerosis. 2011;217(1):268-73. doi: 10.1016/j.atherosclerosis.2011.03.025.
Sumbal A, Sheikh SM, Ikram A, Amir A, Sumbal R, Saeed AR. Latent Tuberculosis Infection (LTBI) as a predictor of coronary artery disease: A systematic review and meta-analysis. Heliyon. 2023;9(4):e15365. doi: 10.1016/j.heliyon.2023.e15365
Li Y, Wu Q, Chen Y. Myocardial infarction and tuberculosis. Acta Cardiol. 2012;67(3):371-2. doi: 10.1080/ac.67.3.2160732.
Majumdar G, Agarwal SK, Pande S, Chandra B, Tewari P. A Case Report of Combined Radical Pericardiectomy and Beating Heart Coronary Artery Bypass Grafting in a Patient with Tubercular Chronic Constrictive Pericarditis with Coronary Artery Disease. Ann Card Anaesth. 2017;20(4):465-7. doi: 10.4103/aca.ACA_102_17.
Farid NA, Jakubowski JA, Payne CD, Li YG, Jin Y, Ernest II CS, et al. Effect of rifampin on the pharmacokinetics and pharmacodynamics of prasugrel in healthy male subjects. Curr Med Res Opin. 2009;25(8):1821-9. doi: 10.1185/03007990903018360.
Teng R, Mitchell P, Butler K. Effect of rifampicin on the pharmacokinetics and pharmacodynamics of ticagrelor in healthy subjects. Eur J Clin Pharmacol. 2013;69(4):877-83. doi: 10.1007/s00228-012-1436-x.
Judge HM, Patil SB, Buckland RJ, Jakubowski JA, Storey RF. Potentiation of clopidogrel active metabolite formation by rifampicin leads to greater P2Y12 receptor blockade and inhibition of platelet aggregation after clopidogrel. J Thromb Haemost JTH.2010;8(8):1820-7. doi: 10.1111/j.1538-7836.2010.03925.x.
Mendell J, Chen S, He L, Desai M, Parasramupria DA. The Effect of Rifampin on the Pharmacokinetics of Edoxaban in Healthy Adults. Clin Drug Investig. 2015;35(7):447-53. doi: 10.1007/s40261-015-0298-2.
Härtter S, Koenen-Bergmann M, Sharma A, Nehmiz G, Lemke U, Timmer W, et al. Decrease in the oral bioavailability of dabigatran etexilate after co-medication with rifampicin. Br J Clin Pharmacol. 2012;74(3):490-500. doi: 10.1111/j.1365-2125.2012.04218.x.
Vakkalagadda B, Frost C, Byon W, Boyd RA, Wang J, Zhang D, et al. Effect of Rifampin on the Pharmacokinetics of Apixaban, an Oral Direct Inhibitor of Factor Xa. Am J Cardiovasc Drugs Drugs Devices Interv. 2016;16(2):119-27. doi: 10.1007/s40256-015-0157-9.
Paul P. Dobesh, Zachary A. Stacy, Chapter 2 - Pharmacology of Oral Anticoagulants. In: Flaker G. Stroke Prevention in Atrial Fibrillation. Elsevier; 2019. p. 11-34. doi: 10.1016/B978-0-323-55429-9.00002-9.
Steffel J, Collins R, Antz M, Cornu P, Desteghe L, Haeusler KG, et al. 2021 European Heart Rhythm Association Practical Guide on the Use of Non-Vitamin K Antagonist Oral Anticoagulants in Patients with Atrial Fibrillation. EP Eur. 2021;23(10):1612-76. doi: 10.1093/europace/euab065.
Lee HJ, Kim HK, Kim BS, Han KD, Park CS, Rhee TM, et al. Safety and effectiveness of anticoagulation with non-vitamin K antagonist oral anticoagulants and warfarin in patients on tuberculosis treatment. Sci Rep. 2023;13:2060. doi: 10.1038/s41598-023-29185-9.
Lobato LS, Rosa PS, Ferreira J da S, Neumann A da S, da Silva MG, do Nascimento DC, et al. Statins Increase Rifampin Mycobactericidal Effect. Antimicrob Agents Chemother. 2014;58(10):5766-74. doi: 10.1128/AAC.01826-13.
Cross GB, Sari IP, Kityo C, Lu Q, Pokharkar Y, Moorakonda RB, et al. Rosuvastatin adjunctive therapy for rifampicin-susceptible pulmonary tuberculosis: a phase 2b, randomised, open-label, multicentre trial. Lancet Infect Dis. 2023;23(7):847-55. doi: 10.1016/S1473-3099(23)00067-1.
Backman JT, Luurila H, Neuvonen M, Neuvonen PJ. Rifampin markedly decreases and gemfibrozil increases the plasma concentrations of atorvastatin and its metabolites. Clin Pharmacol Ther. 2005;78(2):154-67. doi: 10.1016/j.clpt.2005.04.007.
Kyrklund C, Backman JT, Kivistö KT, Neuvonen M, Laitila J, Neuvonen PJ. Rifampin greatly reduces plasma simvastatin and simvastatin acid concentrations. Clin Pharmacol Ther. 2000;68(6):592-7. doi: 10.1067/mcp.2000.111414.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599-726. doi: 10.1093/eurheartj/ehab368.
Agrawal A, Agarwal SK, Kaleekal T, Gupta YK. Rifampicin and antihypertensive drugs in chronic kidney disease: Pharmacokinetic interactions and their clinical impact. Indian J Nephrol. 2016;26(5):322-8. doi: 10.4103/0971-4065.176145.
Liu W, Yan T, Chen K, Yang L, Benet LZ, Zhai S. Predicting Interactions between Rifampin and Antihypertensive Drugs Using the Biopharmaceutics Drug Disposition Classification System. Pharmacotherapy. 2020;40(4):274-90. doi.org/10.1002/phar.2380
Pathways and Guidelines Development Subgroup SACUBITRIL/VALSARTAN (ENTRESTO®) HEART FAILURE INFORMATION FOR PRIMARY CARE [Internet]. Available from: https://gmmmg.nhs.uk/wp-content/uploads/2021/09/Sacubitril-Valsartan-info-sheet-for-GPs-Sep-2021-FINAL.pdf
Kasichayanula S, Liu X, Griffen SC, Lacreta FP, Boulton DW. Effects of rifampin and mefenamic acid on the pharmacokinetics and pharmacodynamics of dapagliflozin. Diabetes Obes Metab. 2013;15(3):280-3. doi: 10.1111/dom.12024.
Macha S, Koenen R, Sennewald R, Schöne K, Hummel N, Riedmaier S, et al. Effect of gemfibrozil, rifampicin, or probenecid on the pharmacokinetics of the SGLT2 inhibitor empagliflozin in healthy volunteers. Clin Ther. 2014;36(2):280-290.e1. doi: 10.1016/j.clinthera.2014.01.003.
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2024 La revista es titular de la primera publicación, luego el autor dando crédito a la primera publicación.

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.

















