Síndrome de Takotsubo: complicación cardiovascular del accidente cerebrovascular
DOI:
https://doi.org/10.47487/apcyccv.v3i4.235Palabras clave:
reporte de caso, accidente cerebrovascular, Infarto agudo de miocardio, fibrilación auricular, síndrome de TakotsuboResumen
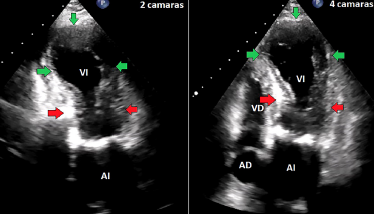
Mujer adulta mayor, 82 años, Katz A, con antecedente de diabetes mellitus tipo 2 e hipertensión arterial; ingresa por accidente cerebrovascular isquémico que se complica con síndrome de Takotsubo con posterior reingreso por fibrilación auricular tras el alta médica. Estos tres eventos clínicos tienen criterios para integrarse como un síndrome cerebro-corazón, el cual es una condición de alto riesgo para mortalidad.
Descargas
Referencias
Scheitz JF, Nolte CH, Doehner W, Hachinski V, Endres M. Stroke–heart syndrome: clinical presentation and underlying mechanisms. Lancet Neurol. 2018;17:1109-20. doi: 10.1016/S1474-4422(18)30336-3.
Sposato LA, Hilz MJ, Aspberg S, Murthy SB, Bahit MC, Hsieh CY, et al; World Stroke Organisation Brain & Heart Task Force. Post-Stroke Cardiovascular Complications and Neurogenic Cardiac Injury: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;76(23):2768-85. doi: 10.1016/j.jacc.2020.10.009.
Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2021;52(7):e364-e467. doi: 10.1161/STR.0000000000000375.
Caprio FZ, Sorond FA. Cerebrovascular Disease: Primary and Secondary Stroke Prevention. Med Clin North Am. 2019;103(2):295- 308. doi: 10.1016/j.mcna.2018.10.001.
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström- Lundqvist C, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021 Feb 1;42(5):373-498. doi: 10.1093/ eurheartj/ehaa612.
Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317-29. doi: 10.1056/ NEJMoa0804656.
Demaerschalk BM, Kleindorfer DO, Adeoye OM, Demchuk AM, Fugate JE, Grotta JC, et al. American Heart Association Stroke Council and Council on Epidemiology and Prevention. Scientific Rationale for the Inclusion and Exclusion Criteria for Intravenous Alteplase in Acute Ischemic Stroke: A Statement for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2016;47(2):581-641. doi: 10.1161/STR.0000000000000086. Erratum in: Stroke. 2016;47(11):e262.
Goldstein DS. The electrocardiogram in stroke: relationship to pathophysiological type and comparison with prior tracings. Stroke. 1979;10(3):253-9. doi: 10.1161/01.str.10.3.253.
Khechinashvili G, Asplund K. Electrocardiographic changes in patients with acute stroke: a systematic review. Cerebrovasc Dis. 2002;14(2):67-76. doi: 10.1159/000064733.
D o e h n e r W, L e i s t n e r D M , A u d e b e r t H J , S c h e i t z J F. T h e r o l e o f c a r d i o l o g i s t s on the stroke unit. Eur Heart J. 2020;22(Supplement_M):M3-M12. doi: 10.1093/eurheartj/suaa160.
Sposato LA, Hilz MJ, Aspberg S, Murthy SB, Bahit MC, Hsieh CY, et al. World Stroke Organisation Brain & Heart Task Force. Post-Stroke Cardiovascular Complications and Neurogenic Cardiac Injury: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;76(23):2768-2785. doi: 10.1016/j.jacc.2020.10.009.
Falk R, Hershberger R. Miocardiopatías dilatada, restrictiva e infiltrante. En: Braunwald’s heart disease: A textbook of cardiovascular medicine. 11th edition. Capítulo 77. Elsevier; 2018. p. 1580-1601.
Collet J, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Deepak L. et al. 2020 ESC Guidelines for themanagement of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42(14):1289-1367. doi: 10.1093/ eurheartj/ehaa575.
Pustjens TFS, Appelman Y, Damman P, Ten Berg JM, Jukema JW, de Winter RJ, et al. Guidelines for the management of myocardial infarction/injury with non-obstructive coronary arteries (MINOCA): a position paper from the Dutch ACS working group. Neth Heart J. 2020;28(3):116-130. doi: 10.1007/s12471-019-01344-6. Erratum in: Neth Heart J. 2020;28(1):59.
Sucato V, Testa G, Puglisi S, Evola S, Galassi AR, Novo G. Myocardial infarction with non-obstructive coronary arteries (MINOCA): Intracoronary imaging-based diagnosis and management. J Cardiol. 2021;77(5):444-451. doi: 10.1016/j.jjcc.2021.01.001.
Kosmas N, Manolis A, Dagres N, Iliodromitis E. Myocardial infarction or acute coronary syndrome with non-obstructive coronary arteries and sudden cardiac death: a missing connection. EP Europace. 2020;22(9):1303-10. doi: 10.1093/europace/euaa156.
Nordenskjöld AM, Agewall S, Atar D, Baron T, Beltrame J, Bergström O, et al. Randomized evaluation of beta blocker and ACE-inhibitor/ angiotensin receptor blocker treatment in patients with myocardial infarction with non-obstructive coronary arteries (MINOCA-BAT): Rationale and design. Am Heart J. 2021;231:96-104. doi: 10.1016/j. ahj.2020.10.059.
Bhatia GS, Lip GY. Atrial fibrillation post-myocardial infarction: frequency, consequences, and management. Curr Heart Fail Rep. 2004;1(4):149-55. doi: 10.1007/s11897-004-0002-y.
Budnik M, Piątkowski R, Ochijewicz D, Zaleska M, Grabowski M, Opolski G. Pathophysiology of Takotsubo Syndrome as A Bridge to Personalized Treatment. J Pers Med. 2021;11(9):879. doi: 10.3390/ jpm11090879.
Goico A, Chandrasekaran M, Herrera CJ. Novel developments in stress cardiomyopathy: From pathophysiology to prognosis. Int J Cardiol. 2016;223:1053-1058. doi: 10.1016/j.ijcard.2016.08.241.
Johnson NP, Chavez JF, Mosley WJ 2nd, Flaherty JD, Fox JM. Performance of electrocardiographic criteria to differentiate Takotsubo cardiomyopathy from acute anterior ST elevation myocardial infarction. Int J Cardiol. 2013;164(3):345-8. doi: 10.1016/j.ijcard.2011.07.029.
Kosuge M, Kimura K. Electrocardiographic findings of takotsubo cardiomyopathy as compared with those of anterior acute myocardial infarction. J Electrocardiol. 2014;47(5):684-9. doi: 10.1016/j.jelectrocard.2014.03.004.
Akashi YJ, Nef HM, Lyon AR. Epidemiology and pathophysiology of Takotsubo syndrome. Nat Rev Cardiol. 2015;12(7):387-97. doi: 10.1038/nrcardio.2015.39.
Ghadri JR, Kato K, Cammann VL, Gili S, Jurisic S, Di Vece D, et al. Long-Term Prognosis of Patients With Takotsubo Syndrome. J Am Coll Cardiol. 2018;72(8):874-882. doi: 10.1016/j.jacc.2018.06.016.
Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu D, Jaguszewski M, et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med. 2015;373(10):929-938. doi: 10.1056/nejmoa1406761.
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2022 La revista es titular de la primera publicación, luego el autor dando crédito a la primera publicación.

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.