Comparison of the epidemiological, clinical and diagnostic characteristics of infective endocarditis of native and prosthetic valves in a Peruvian reference center
DOI:
https://doi.org/10.47487/apcyccv.v6i1.463Keywords:
Endocarditis, Diagnosis , Signs and Symptoms, PeruAbstract
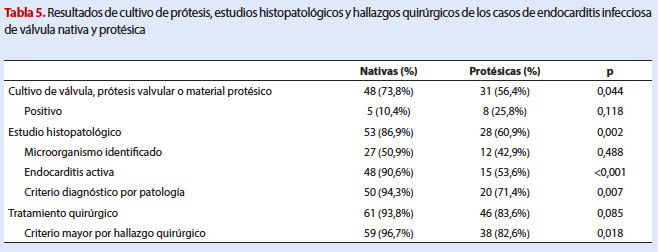
Objective. To compare the epidemiological, clinical and diagnostic characteristics of patients with native valve infective endocarditis (NVIE) and prosthetic valve infective endocarditis (PVIE) treated in a Peruvian reference center. Materials and methods. A retrospective, descriptive study was conducted on patients diagnosed with NVIE and PVIE at the Instituto Nacional Cardiovascular (INCOR), EsSalud, between 2017 and 2023. Results. A total of 65 NVIE and 55 PVIE cases were identified, with community-acquired infections predominating (92.3% in NVIE, 83.6% in PVIE). PVIE patients were older (mean age: 63.7 vs. 46.1 years, p<0.001) and had more comorbidities. The key predisposing factor in PVIE was prior endocarditis (20.0%) and valve repair (14.5%), while congenital heart disease (41.5%) and valvular disease (21.5%) predominated in NVIE. Fever and dyspnea were the most common symptoms in both groups. The aortic valve was the most frequently affected (78.5% in NVIE, 87.3% in PVIE). NVIE was associated with vegetation (92.3%) and leaflet perforations (41.5%), while PVIE showed more abscesses (34.5%) and pseudoaneurysms (36.4%). Cardiac computed tomography identified vegetations and pseudoaneurysms in both groups. Blood cultures were positive in 49.2% of NVIE and 65.5% of PVIE, with Streptococcus species predominant in NVIE and Staphylococcus species in PVIE. Surgical treatment was performed in 96.7% of NVIE and 82.6% of PVIE cases. Conclusions. NVIE predominantly affected younger patients with congenital heart disease, while PVIE was more common in older patients with comorbidities. Transesophageal echocardiography and microbiological findings were essential for diagnosis.
Downloads
References
Li M, Kim JB, Sastry BKS, Chen M. Infective endocarditis. Lancet. julio de 2024;404(10450):377-92. doi: 10.1016/S0140-6736(24)01098-5.
Kamde SP, Anjankar A. Pathogenesis, Diagnosis, Antimicrobial Therapy, and Management of Infective Endocarditis, and Its Complications. Cureus. 2022 Sep 15;14(9):e29182. doi: 10.7759/cureus.29182.
Habib G, Erba PA, Iung B, Donal E, Cosyns B, Laroche C, et al. Clinical presentation, aetiology and outcome of infective endocarditis. Results of the ESC-EORP EURO-ENDO (European infective endocarditis) registry: a prospective cohort study. Eur Heart J. 2019;40(39):3222-3232. doi: 10.1093/eurheartj/ehz620.
Delgado V, Ajmone Marsan N, De Waha S, Bonaros N, Brida M, Burri H, et al. 2023 ESC Guidelines for the management of endocarditis. Eur Heart J. 2023;44(39):3948-4042. doi: 10.1093/eurheartj/ehad193.
Dayer MJ, Quintero-Martinez JA, Thornhill MH, Chambers JB, Pettersson GB, Baddour LM. Recent Insights Into Native Valve Infective Endocarditis. J Am Coll Cardiol. 2024;83(15):1431-1443. doi: 10.1016/j.jacc.2023.12.043.
Cuervo G, Quintana E, Regueiro A, Perissinotti A, Vidal B, Miro JM, et al. The Clinical Challenge of Prosthetic Valve Endocarditis. J Am Coll Cardiol. 2024;83(15):1418-1430. doi: 10.1016/j.jacc.2024.01.037.
Van Der Vaart TW, Bossuyt PMM, Durack DT, Baddour LM, Bayer AS, Durante-Mangoni E, et al. External Validation of the 2023 Duke–International Society for Cardiovascular Infectious Diseases Diagnostic Criteria for Infective Endocarditis. Clin Infect Dis. 2024;78(4):922-929. doi: 10.1093/cid/ciae033.
Yang X, Chen H, Zhang D, Shen L, An G, Zhao S. Global magnitude and temporal trend of infective endocarditis, 1990–2019: results from the Global Burden of Disease Study. Eur J Prev Cardiol. 2022;29(8):1277-1286. doi: 10.1093/eurjpc/zwab184.
Bea C, Vela S, García-Blas S, Perez-Rivera JA, Díez-Villanueva P, De Gracia AI, et al. Infective Endocarditis in the Elderly: Challenges and Strategies. J Cardiovasc Dev Dis. 2022;9(6):192. doi: 10.3390/jcdd9060192.
Seguel S. E, Rojas-Campillay C, Peralta-Jiménez GA, Hernández-Paredes F, Vera-Calzaretta A, González L. R, et al. Cambios en el perfil epidemiológico de la Endocarditis Infecciosa con indicación quirúrgica entre 1983 y 2020. Rev Méd Chile. septiembre de 2023;151(9):1185-93. doi: 10.4067/s0034-98872023000901185.
Polo Lecca GDC, Torres-Villacorta L, Yarahuaman-Mora J, Lobato-Jeri C, Uribe-Badillo E. Experiencia de cinco años en el manejo de endocarditis infecciosa complicada en un centro de referencia nacional. Arch Peru Cardiol Cir Cardiovasc. 2023;1(3):151-156. Spanish. doi: 10.47487/apcyccv.v1i3.77.
Jussli-Melchers J, Salem MA, Schoettler J, Friedrich C, Huenges K, Elke G, et al. Mid- and Long-Term Surgical Outcomes Due to Infective Endocarditis in Elderly Patients: A Retrospective Cohort Study. J Clin Med. 2022;11(22):6693. doi: 10.3390/jcm11226693.
Ostovar R, Zinab FS, Schröter F, Hartrumpf M, Fritzsche D, Albes JM. Does Age Influence the Preoperative Condition and, Thus, the Outcome in Endocarditis Patients? J Clin Med. 2023;12(3):822. doi: 10.3390/jcm12030822.
Lasso Maldonado CC, Guerra Romero HA, Olivera Gamarra MC, Orozco Sotomayor SP, Brito Jacome CJ, Cárdenas Vásquez DC, et al. Mortalidad de la Endocarditis Infecciosa en los Últimos 5 años. Ciencia Latina. 2024;8(2):322-37. doi: https://doi.org/10.37811/cl_rcm.v8i2.10440.
Budea C, Bratosin F, Bogdan I, Bota A, Turaiche M, Tirnea L, et al. Clinical Presentation and Risk Factors of Infective Endocarditis in the Elderly: A Systematic Review. J Pers Med. 2023;13(2):296. doi: 10.3390/jpm13020296.
Cecchi E, Imazio M, De Rosa FG, Chirillo F, Enia F, Pavan D, et al. Infective endocarditis in the real world: the Italian Registry of Infective Endocarditis (Registro Italiano Endocardite Infettiva – RIEI). J Cardiovasc Med (Hagerstown). 2008;9(5):508-14. doi: 10.2459/JCM.0b013e3282f20ae6.
Ramos-Martínez A, Domínguez F, Muñoz P, Marín M, Pedraz Á, Fariñas MC, et al. Clinical presentation, microbiology, and prognostic factors of prosthetic valve endocarditis. Lessons learned from a large prospective registry. PLoS One. 2023;18(9):e0290998. doi: 10.1371/journal.pone.0290998.
Kazelian LR, Gagliardi JA, Llobera MEN, Lespada MI, Beck MA, Cianciulli TF. Experiencia en endocarditis infecciosa a lo largo de 30 años en un hospital de Buenos Aires. Medicina (Buenos Aires). 2021;81(6):939-945.
Slouha E, Al-Geizi H, Albalat BR, Burle VS, Clunes LA, Kollias TF. Sex Differences in Infective Endocarditis: A Systematic Review. Cureus. 2023;15(12):e49815. doi: 10.7759/cureus.49815.
Salim HT, Hamad YA, Alwadiya H, Siriya W, Mansour B, Alhadad H, et al. Sex-specific differences in infective endocarditis: A systematic review and meta-analysis of clinical profiles and management outcomes. Int J Cardiol Heart Vasc. 2025;56:101607. doi: 10.1016/j.ijcha.2025.101607.
Mettler SK, Alhariri H, Okoli U, Charoenngam N, Guillen RH, Jaroenlapnopparat A, et al. Gender, Age, and Regional Disparities in the Incidence and Mortality Trends of Infective Endocarditis in the United States Between 1990 and 2019. Am J Cardiol. 2023;203:128-135. doi: 10.1016/j.amjcard.2023.07.018.
Havers-Borgersen E, Østergaard L, Holgersson CK, Stahl A, Schmidt MR, Smerup M, et al. Infective endocarditis with or without congenital heart disease: clinical features and outcomes. Eur Heart J. 2024;45(44):4704-4715. doi: 10.1093/eurheartj/ehae548.
Carvajal V, Reyes FB, Gonzalez D, Schwartz M, Whiltlow A, Alegria JR. Endocarditis in Adult Congenital Heart Disease Patients: Prevention, Recognition, and Management. Curr Cardiol Rep. 2024;26(9):1031-1045. doi: 10.1007/s11886-024-02103-9.
Caselli S, Attenhofer Jost C, Greutmann M. Infective endocarditis in congenital heart disease: the expected and the unexpected. Eur Heart J. 2024;45(44):4716-4718. doi: 10.1093/eurheartj/ehae603.
Bezerra RL, Salgado LS, Silva YMD, Figueiredo GGR, Bezerra RM, Machado ELG, et al. Epidemiological Profile of Patients with Infective Endocarditis at three Tertiary Centers in Brazil from 2003 to 2017. Int J Cardiovasc Sci. 2022;35(4):467-75. doi: 10.36660/ijcs.20210181.
Perez-Rivera JA, Armiñanzas C, Muñoz P, Kestler M, Pinilla B, Fariñas MC, et al. Comorbidity and Prognosis in Octogenarians with Infective Endocarditis. J Clin Med. 2022 Jun 29;11(13):3774. doi: 10.3390/jcm11133774.
Ariza EJ, Suárez EU, Giraldo S, Jaimes FA, Muñoz E, Senior JM. Características epidemiológicas de la endocarditis infecciosa. Experiencia de seis años. Rev Colomb Cardiol. 2022;29(4):441-448. doi: 10.24875/rccar.21000059.
Østergaard L, Voldstedlund M, Bruun NE, Bundgaard H, Iversen K, Køber N, et al. Temporal Changes, Patient Characteristics, and Mortality, According to Microbiological Cause of Infective Endocarditis: A Nationwide Study. J Am Heart Assoc. 2022;11(16):e025801. doi: 10.1161/JAHA.122.025801.
Reisinger M, Kachel M, George I. Emerging and Re-Emerging Pathogens in Valvular Infective Endocarditis: A Review. Pathogens. 2024;13(7):543. doi: 10.3390/pathogens13070543.
Fowler VG, Durack DT, Selton-Suty C, Athan E, Bayer AS, Chamis AL, et al. The 2023 Duke-International Society for Cardiovascular Infectious Diseases Criteria for Infective Endocarditis: Updating the Modified Duke Criteria. Clin Infect Dis. 2023;77(4):518-526. doi: 10.1093/cid/ciad271.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 The journal is headline of the first publication, then the author giving credit to the first publication.

This work is licensed under a Creative Commons Attribution 4.0 International License.














