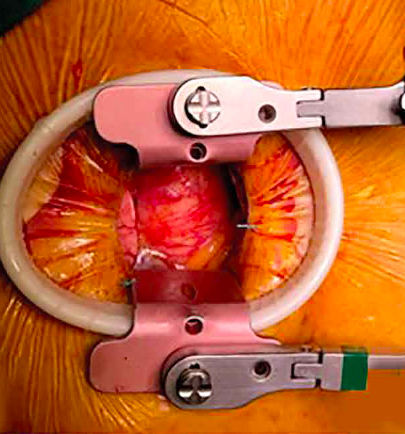
Aortic valve replacement through minithoracotomy. Results from the Peruvian experience
DOI:
https://doi.org/10.47487/apcyccv.v3i2.219Palabras clave:
Aortic valve, Thoracotomy, Cardiac Surgery, PeruResumen
Objectives. To assess mortality, major valve-related events (MAVRE), and other complications in the perioperative period and follow up in patients with aortic valve replacement (AVR) through minithoracotomy (MT). Methods. We retrospectively analyzed patients aged <80 who underwent AVR through MT between January 2017 and December 2021 in a national reference center in Lima, Peru. Patients undergoing other surgical approaches (mini-sternotomy, etc.), other concomitant cardiac procedures, redo, and emergency surgeries were excluded. We measured the variables (MAVRE, mortality, and other clinical variables) at 30 days and a mean follow-up of 12 months. Results. Fifty-four patients were studied, the median age was 69.5 years, and 65% were women. Aortic valve (AV) stenosis was the main indication for surgery (65%), and bicuspid AV represented 55.6% of cases. At 30-days, MAVRE occurred in two patients (3.7%), with no in-hospital mortality. One patient had an intraoperative ischemic stroke, and one required a permanent pacemaker. No patient underwent reoperation due to prosthesis dysfunction or endocarditis. In a mean follow-up of one year, MAVRE occurrence did not show variations with the perioperative period, most patients remained in NYHA I (90.7%) or II (7.4%) compared to the preoperative period (p<0.001). Conclusions. AV replacement through MT is a safe procedure in our center for patients under 80 years.
Descargas
Referencias
Iung B, Delgado V, Rosenhek R, Price S, Prendergast B, Wendler O, et al. Contemporary presentation and management of valvular heart disease: The EURObservational Research Programme Valvular Heart Disease II Survey. Circulation. 2019;140(14):1156-1169. doi: 10.1161/CIRCULATIONAHA.119.041080.
Yadgir S, Johnson CO, Aboyans V, Adebayo OM, Adedoyin RA, Afarideh M, et al. Global, regional, and national burden of
calcific aortic valve and degenerative mitral valve diseases, 1990-2017. Circulation. 2020;141(21):1670-1680. doi: 10.1161/CIRCULATIONAHA.119.043391.
Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the Task Force for the management of valvular heart disease. Eur Heart J. 2022;43(7):561-632. doi: 10.1093/eurheartj/ehab395.
Losanoff JE, Richman BW, Jones JW. Disruption and infection of median sternotomy: a comprehensive review. Eur J Cardiothorac Surg. 2002;21(5):831-9. doi: 10.1016/s1010-7940(02)00124-0.
Huang AP, Sakata RK. Pain after sternotomy - review. Braz J Anesthesiol. 2016;66(4):395-401. doi: 10.1016/j.bjane.2014.09.013.
King KM, McFetridge-Durdle J, LeBlanc P, Anzarut A, Tsuyuki RT. A Descriptive Examination of the Impact of Sternal Scar Formation in Women. Eur J Cardiovasc Nurs. 2009;8(2):112-118. doi: 10.1016/j.ejcnurse.2008.08.001
İyigün T, Kaya M, Gülbeyaz SÖ, Fıstıkçı N, Uyanık G, Yılmaz B, et al. Patient body image, self-esteem, and cosmetic results of minimally invasive robotic cardiac surgery. Int J Surg. 2017;39:88-94. doi: 10.1016/j.ijsu.2017.01.105.
Svensson LG. Minimal-access “J” or “j” sternotomy for valvular, aortic, and coronary operations or reoperations. Ann Thorac Surg. 1997;64(5):1501-3. doi: 10.1016/S0003-4975(97)00927-2.
Moreno-Cabral RJ. Mini-T sternotomy for cardiac operations. J Thorac Cardiovasc Surg. 1997;113(4):810-1. doi: 10.1016/S0022-5223(97)70252-6.
Akins CW, Miller DC, Turina MI, Kouchoukos NT, Blackstone EH, Grunkemeier GL, et al. Guidelines for reporting mortality and morbidity after cardiac valve interventions. J Thorac Cardiovasc Surg. 2008;135(4):732-8. doi: 10.1016/j.jtcvs.2007.12.002.
Bevan GH, Zidar DA, Josephson RA, Al-Kindi SG. Mortality Due to Aortic Stenosis in the United States, 2008-2017. JAMA. 2019;321(22):2236-2238. doi: 10.1001/jama.2019.6292.
Powell R, Pelletier MP, Chu MWA, Bouchard D, Melvin KN, Adams C. The Perceval Sutureless Aortic Valve: Review of Outcomes, Complications, and Future Direction. Innovations (Phila). 2017;12(3):155-173. doi: 10.1097/IMI.0000000000000372.
Glauber M, Ferrarini M, Miceli A. Minimally invasive aortic valve surgery: state of the art and future directions. Ann Cardiothorac Surg. 2015;4(1):26-32. doi: 10.3978/j.issn.2225-319X.2015.01.01.
Phan K, Xie A, Di Eusanio M, Yan TD. A meta-analysis of minimally invasive versus conventional sternotomy for aortic valve replacement. Ann Thorac Surg. 2014;98(4):1499-511. doi: 10.1016/j.athoracsur.2014.05.060.
Brown ML, McKellar SH, Sundt TM, Schaff HV. Ministernotomy versus conventional sternotomy for aortic valve replacement: a systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2009;137(3):670-679.e5. doi: 10.1016/j.jtcvs.2008.08.010.
Ariyaratnam P, Loubani M, Griffin SC. Minimally invasive aortic valve replacement: Comparison of long-term outcomes. Asian Cardiovasc Thorac Ann. 2015;23(7):814-21. doi: 10.1177/0218492315587606.
Chang C, Raza S, Altarabsheh SE, Delozier S, Sharma UM, Zia A, et al. Minimally Invasive Approaches to Surgical Aortic Valve Replacement: A Meta-Analysis. Ann Thorac Surg. 2018;106(6):1881-1889. doi: 10.1016/j.athoracsur.2018.07.018.
Yousuf Salmasi M, Hamilton H, Rahman I, Chien L, Rival P, Benedetto U, et al, Vohra HA. Mini-sternotomy vs right anterior thoracotomy for aortic valve replacement. J Card Surg. 2020;35(7):1570-1582. doi: 10.1111/jocs.14607.
Fortunato J, Jeronimo A, Sesca J, Paludo R, Paz M, Paludo L, et al. Troca valvar aórtica minimamente invasiva: uma alternativa à técnica convencional. Braz J Cardiovasc Surg. 2012;27(4):570-582. doi: 10.5935/1678-9741.20120099.
Benetti F, Rizzardi JL, Concetti C, Bergese M, Zappetti A. Minimally aortic valve surgery avoiding sternotomy. Eur J Cardiothorac Surg. 1999;16 Suppl 2:S84-5.
Publicado
Número
Sección
Licencia
Derechos de autor 2022 La revista es titular de la primera publicación, luego el autor dando crédito a la primera publicación.

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.

















