Monitoreo hemodinámico invasivo por catéter de arteria pulmonar Swan-Ganz: conceptos y utilidad
DOI:
https://doi.org/10.47487/apcyccv.v2i3.152Palabras clave:
Hipertensión pulmonar, Monitoreo hemodinámico, Choque cardiogénico, Insuficiencia cardiacaResumen
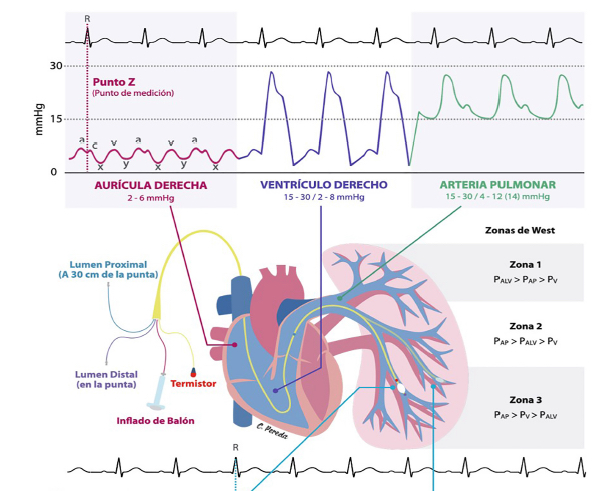
Desde sus inicios en el siglo pasado, el cateterismo de arteria pulmonar (CAP) ha ido evolucionando hasta ser una técnica de evaluación hemodinámica invasiva que puede realizarse en la cama del paciente a través de un catéter Swan-Ganz; este procedimiento ha mantenido un curso intermitente en cuanto a su uso; no obstante, actualmente ha demostrado relevancia en escenarios específicos. El CAP permite el acceso a la circulación venosa central, el corazón derecho y la arteria pulmonar; realiza el cálculo de variables hemodinámicas de manera directa o indirecta mediante fórmulas y métodos establecidos. Esto hace posible realizar una evaluación y clasificación hemodinámica adecuada, realizar pruebas específicas (p. ej. prueba de vasorreactividad), que ayudan a definir el diagnóstico, la conducta terapéutica, monitorizar la respuesta al tratamiento, la evaluación previa a terapias avanzadas (p. ej. el trasplante cardiaco o dispositivos de asistencia circulatoria mecánica), y el pronóstico en los pacientes. En este artículo profundizamos sobre los conceptos y la utilidad del cateter de arteria pulmonar.
Descargas
Referencias
Hsu S, Fang JC, Borlaug BA. Hemodynamics for the Heart Failure Clinician: A State-of-the-Art Review. J Card Fail. 2021;S1071-9164(21)00306-7. doi:10.1016/j.cardfail.2021.07.012
Lategola M, Rahn H. A self-guiding catheter for cardiac and pulmonary arterial catheterization and occlusion. Proc Soc Exp Biol Med. 1953;84(3):667-668. doi:10.3181/00379727-84-20745
Swan HJ, Ganz W, Forrester J, Marcus H, Diamond G, Chonette D. Catheterization of the heart in man with use of a flow-directed balloon-tipped catheter. N Engl J Med. 1970;283(9):447–51. doi:10.1056/NEJM197008272830902.
Forrester JS. A Tale of Serendipity, Ingenuity, and Chance: 50th Anniversary of Creation of the Swan-Ganz Catheter. J Am Coll Cardiol. 2019;74(1):100-103. doi:10.1016/j.jacc.2019.04.050.
Binanay C, Califf RM, Hasselblad V, O’Connor CM, Shah MR, Sopko G, et al. Evaluation study of congestive heart failure and pulmonary artery catheterization effectiveness: the ESCAPE trial. JAMA. 2005;294(13):1625–33. doi:10.1001/jama.294.13.1625.
Isseh IN, Lee R, Khedraki R, Hoffman K. A Critical Review of Hemodynamically Guided Therapy for Cardiogenic Shock: Old Habits Die Hard. Curr Treat Options Cardiovasc Med. 2021;23(5):29. doi:10.1007/s11936-021-00903-8.
Doshi R, Patel H, Shah P. Pulmonary artery catheterization use and mortality in hospitalizations with HFrEF and HFpEF: A nationally representative trend analysis from 2005 to 2014. Int J Cardiol. 2018;269:289-291. doi:10.1016/j.ijcard.2018.07.069
Saxena A, Garan AR, Kapur NK, O’Neill WW, Lindenfeld J, Pinney S, et al. Value of Hemodynamic Monitoring in Patients With Cardiogenic Shock Undergoing Mechanical Circulatory Support. Circulation. 2020;141(14):1184-1197. doi:10.1161/CIRCULATIONAHA.119.043080
Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E. Braunwald’s heart disease, a textbook of cardiovascular medicine. 11th ed. Philadelphia: Elsevier Inc; 2019.
García X, Mateu L, Maynar J, Mercadal J, Ochagavía A, Ferrandiz A. Estimación del gasto cardíaco. Utilidad en la práctica clínica. Monitorización disponible invasiva y no invasiva. Medicina Intensiva. 2011; 35(9): 552 - 561. Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0210-56912011000900004&lng=es
Madias C, Kimmelstiel C. (2017) Right Heart Catheterization. In: Hendel R., Kimmelstiel C. (eds) Cardiology Procedures. Springer, London. doi: 10.1007/978-1-4471-7290-1_14.
Mueller HS, Chatterjee K, Davis KB, Fifer MA, Franklin C, Greenberg MA, et al. ACC expert consensus document. Present use of bedside right heart catheterization in patients with cardiac disease. American College of Cardiology. J Am Coll Cardiol. 1998;32(3):840-864. doi:10.1016/s0735-1097(98)00327-1
Griffin BP, Topol EJ, editors. Manual of cardiovascular medicine. 5th ed. Philadelphia: Lippincott Williams and Wilkins; 2018.
Moscucci M. Grossman & Baim’s Cardiac catheterization, angiography and intervention. Philadelphia Lippincott Williams and Wilkins 9th ed. 2020.
Sorajja P, Lim MJ, Kern MJ. Kern’s cardiac catheterization handbook. 7th ed. Oxford, Elsevier Health Sciences, 2019.
Kapur NK, Esposito ML, Bader Y, Morine KJ, Kiernan MS, Pham DT, et al. Mechanical Circulatory Support Devices for Acute Right Ventricular Failure. Circulation. 2017;136(3):314-326. doi:10.1161/CIRCULATIONAHA.116.025290
Pellegrini P, Rossi A, Pasotti M, Raineri C, Cicoira M, Bonapace S, et al. Prognostic relevance of pulmonary arterial compliance in patients with chronic heart failure. Chest. 2014;145(5):1064-1070. doi:10.1378/chest.13-1510
Tampakakis E, Shah SJ, Borlaug BA, Leavy PJ, Patel HH, Miller WL, et al. Pulmonary Effective Arterial Elastance as a Measure of Right Ventricular Afterload and Its Prognostic Value in Pulmonary Hypertension Due to Left Heart Disease. Circ Heart Fail. 2018;11(4):e004436. doi:10.1161/CIRCHEARTFAILURE.117.004436.
Mazimba S, Welch TS, Mwansa H, Breathett KK, Kennedy JL, Mihalek AD, et al. Haemodynamically Derived Pulmonary Artery Pulsatility Index Predicts Mortality in Pulmonary Arterial Hypertension. Heart Lung Circ. 2019;28(5):752-760. doi:10.1016/j.hlc.2018.04.280
Kang G, Ha R, Banerjee D. Pulmonary artery pulsatility index predicts right ventricular failure after left ventricular assist device implantation. J Heart Lung Transplant. 2016;35(1):67-73. doi:10.1016/j.healun.2015.06.009.
D’Alto M, Dimopoulos K, Coghlan JG, Kovacs G, Rosenkranz S, Naeije R. Right Heart Catheterization for the Diagnosis of Pulmonary Hypertension: Controversies and Practical Issues. Heart Fail Clin. 2018;14(3):467-477. doi:10.1016/j.hfc.2018.03.011
Aschauer S, Kammerlander AA, Zotter-Tufaro C, Ristl R, Pfaffenberger S, Bachmann A, et al. The right heart in heart failure with preserved ejection fraction: insights from cardiac magnetic resonance imaging and invasive haemodynamics. Eur J Heart Fail. 2016;18(1):71-80. doi:10.1002/ejhf.418.
Condon DF, Nickel NP, Anderson R, Mirza S, de Jesus Perez VA. The 6th World Symposium on Pulmonary Hypertension: what’s old is new. F1000Res. 2019;8:F1000 Faculty Rev-888. Published 2019 Jun 19. doi:10.12688/f1000research.18811.1
Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67-119. doi:10.1093/eurheartj/ehv317
Ragosta, Michael. Textbook of Clinical Hemodynamics E-Book. Elsevier Health Sciences, 2017.
Drazner MH, Velez-Martinez M, Ayers CR, Reimold SC, Thibodeau JT, Mishkin JD, et al. Relationship of right- to left-sided ventricular filling pressures in advanced heart failure: insights from the ESCAPE trial. Circ Heart Fail. 2013;6(2):264-270. doi:10.1161/CIRCHEARTFAILURE.112.000204
Vachiéry J-L, Tedford RJ, Rosenkranz S, Palazzini M, Lang I, Guazzi M, et al. Pulmonary hypertension due to left heart disease. Eur Respir J 2019; 53: 1801897
Simonneau G, Montani D, Celermajer DS, Denton CP, Gatzoulis MA, Krowka M, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J 2019; 53: 1801913.
Arman T. Askari, Adrian W. Messerli. Cardiovascular Hemodynamics. USA: Human Press, 2019.
Iyad N, Ran L, Rola K, Hoffman K. A Critical Review of Hemodynamically Guided Therapy for Cardiogenic Shock: Old Habits Die Hard. Curr Treat Options Cardio Med. 2021; 23: 29.
Siddiqi UA, Belkin M, Kalantari S, Kanelidis A, Miller T, Sarswat N, et al. Prognostic Role of Simultaneous Assessment of Biventricular Function Using Left Ventricular Stroke Work Index and Right Ventricular Stroke Work Index.J Heart Lung Transplant. 2021;40(4):S262.doi: 10.1016/j.healun.2021.01.747
Rosenkranz S, Preston IR. Right heart catheterization: best practice and pitfalls in pulmonary hypertension. Eur Respir Rev. 2015;24(138):642-652. doi:10.1183/16000617.0062-2015
Van Diepen S, Katz JN, Albert NM, Henry TD, Jacobs AK, Kapur NK, et al. Contemporary Management of Cardiogenic Shock: A Scientific Statement From the American Heart Association. Circulation. 2017;136(16):e232-e268. doi:10.1161/CIR.0000000000000525.
Tehrani BN, Truesdell AG, Sherwood MW, Desai S, Tran HA, Epps KC, et al. Standardized Team-Based Care for Cardiogenic Shock. J Am Coll Cardiol. 2019;73(13):1659-1669. doi:10.1016/j.jacc.2018.12.084.
Hernandez GA, Lemor A, Blumer V, et al. Trends in Utilization and Outcomes of Pulmonary Artery Catheterization in PH With and Without Cardiogenic Shock. Journal of Cardiac Failure. 2019;25(5):364-371. doi:10.1016/j.cardfail.2019.03.004.
Garan AR, Kanwar M, Thayer KL, Whitehead E, Zweck E, Hernandez-Montfort J, et al. Complete Hemodynamic Profiling With Pulmonary Artery Catheters in Cardiogenic Shock Is Associated With Lower In-Hospital Mortality. JACC Heart Fail. 2020;8(11):903-913. doi:10.1016/j.jchf.2020.08.012.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Rev Esp Cardiol (Engl Ed). 2016;69(12):1167. doi:10.1016/j.rec.2016.11.005
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):e240-e327. doi:10.1161/CIR.0b013e31829e8776
Kohsaka, S, Menon V, Lowe AP, Lange M, Dzavik V, Sleeper LA, et al. (2005). Systemic Inflammatory Response Syndrome After Acute Myocardial Infarction Complicated by Cardiogenic Shock. Archives of Internal Medicine, 165(14), 1643. https://doi.org/10.1001/archinte.165.14.1643
Ranka S, Mastoris I, Kapur NK, Tedford R, Rali A, Acharya P, et al. Right Heart Catheterization in Cardiogenic Shock Is Associated With Improved Outcomes: Insights From the Nationwide Readmissions Database. J Am Heart Assoc. 2021;e019843. doi:10.1161/JAHA.120.019843.
Osman M, Syed M, Patel B, Munir MB, Kheiri B, Caccamo M, et al. Invasive Hemodynamic Monitoring in Cardiogenic Shock Is Associated With Lower In-Hospital Mortality. J Am Heart Assoc. 2021;10(18):e021808. doi:10.1161/JAHA.121.021808
Khera R, Pandey A, Kumar N, Singh R, Bano S, Golwala H, et al. Variation in Hospital Use and Outcomes Associated With Pulmonary Artery Catheterization in Heart Failure in the United States. Circ Heart Fail. 2016;9(11):e003226. doi:10.1161/CIRCHEARTFAILURE.116.003226
Borlaug BA. Evaluation and management of HFpEF. Nat Rev Cardiol. 2020;17(9):559-573. doi:10.1038/s41569-020-0363-2
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;ehab368. doi:10.1093/eurheartj/ehab368.
Wang W, Cheung A, Watson TJ, Ong PJ, Tcheng JE. Mechanical Complications of Acute Myocardial Infraction. In: Watson TJ, Ong PJL, Tcheng JE, eds. Primary Angioplasty: A Practical Guide. Singapore: Springer; July 14, 2018.275-287.
Ikuta K, Wang Y, Robinson A, Ahmad T, Krumholz HM, Desai NR. National trends in use and outcomes of pulmonary artery catheters among Medicare beneficiaries, 1999–2013. JAMA Cardiol. 2017;2(8):908–13. doi:10.1001/jamacardio.2017.1670.
Potapov EV, Antonides C, Crespo-Leiro MG, Combes A, Färber G, Hannan MM, et al. 2019 EACTS Expert Consensus on long-term mechanical circulatory support. Eur J Cardiothorac Surg. 2019;56(2):230-270. doi:10.1093/ejcts/ezz098.
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2021 La revista es titular de la primera publicación, luego el autor dando crédito a la primera publicación.

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.

















