Revascularización en disfunción del ventrículo izquierdo
DOI:
https://doi.org/10.47487/apcyccv.v2i1.112Palabras clave:
disfunción del ventrículo izquierdo, viabilidad, Revascularización miocárdicaResumen
La disfunción del ventrículo izquierdo por remodelación adversa constituye la condición anatómica estructural subyacente de la insuficiencia cardíaca y es la secuela principal, y más severa, de la enfermedad arterial coronaria a largo plazo; además, es la única patología que se puede beneficiar con la revascularización miocárdica quirúrgica. Para su control existen guías actuales de tratamiento médico sustentados en los resultados favorables de ensayos clínicos contemporáneos. Sin embargo, en estudios recientes, no hubo beneficio de la revascularización quirúrgica sumada a la terapia médica óptima al compararse con la terapia médica óptima sola. La identificación de la viabilidad miocárdica para guiar la revascularización tampoco fue favorable. Los resultados de la extensión de estos ensayos evidenciaron beneficio del tratamiento de revascularización, pero la detección de viabilidad permaneció sin ser favorable. El aumento de la fracción de eyección del ventrículo izquierdo, como marcador de beneficio de la revascularización, no se asoció con menor mortalidad. Existen muchas razones por las cuales las ventajas conocidas de la revascularización no fueron evidenciadas. A pesar de estas discrepancias, la revascularización miocárdica y la identificación de viabilidad en estos pacientes tienen sustento y suelen ser indicaciones de tratamiento habituales.
Descargas
Referencias
Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 2016; 133(4):e38-360.
Anavekar NS, Chareonthaitawee P, Narula J, Gersh BJ. Revascularization in patients with severe left ventricular dysfunction: is the assessment of viability still viable? J Am Coll Cardiol 2016;67:2874-87.
Armstrong PW. Left ventricular dysfunction: causes, natural history, and hopes for reversal. Heart 2000;84 Suppl 1:i15-7.
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2016;18: 891-975.
Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/ AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol 2017;70:776-803.
Cohn JN, Ferrari R, Sharpe N. Cardiac remodeling-concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. On behalf of an International Forum on Cardiac Remodeling. J Am Coll Cardiol 2000;35:569-82.
Aimo A, Gaggin HK, Barison A, Emdin M, Januzzi JL, et al. Imaging, biomarker, and clinical predictors of cardiac remodeling in heart failure with reduced ejection fraction. J Am Coll Cardiol HF 2019;7:782-94.
Halliday BP, Wassall R, Lota AS, et al. Withdrawal of pharmacological treatment for heart failure in patients with recovered dilated cardiomyopathy (TRED-HF): an open-label, pilot, randomised trial. Lancet 2019;393:61-73.
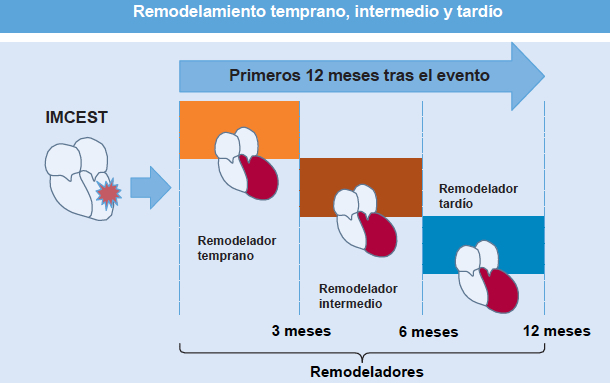
Van der Bijl P, Abou R, Goedemans L, et al. Left ventricular post-infarct remodeling. Implications for systolic function improvement and outcomes in the modern era. J Am Coll Cardiol HF 2020;8:131-40.
Koitabashi N, Kass DA. Reverse remodeling in heart failure-mechanisms and therapeutic opportunities. Nat Rev Cardiol 2011;9:147-57.
Chareonthaitawee P, Gersh BJ, Araoz PA, Gibbons RJ. Revascularization in severe left ventricular dysfunction: the role of viability testing. J Am Coll Cardiol 2005;46:567-74.
Underwood SR, Bax JJ, vom Dahl J, et al. Imaging techniques for the assessment of myocardial hibernation. Report of a Study Group of the European Society of Cardiology. Eur Heart J 2004;25:815-36.
Rahimtoola SH. A perspective on the three large multicenter randomized clinical trials of coronary bypass surgery for chronic stable angina. Circulation 1985;72: V123-V135.
Braunwald E, Kloner RA. The stunned myocardium: prolonged, postischemic ventricular dysfunction. Circulation 1982;66:1146-9.
Kim SJ, Depre C, Vatner S. Novel mechanisms mediating stunned myocardium. Heart Fail Rev 2003;8:143-53.
Gibb AA, Hill BG. Metabolic coordination of physiological and pathological cardiac remodeling. Circ Res 2018;123:107-28.
Shah BN, Khattar RS, Senior R. The hibernating myocardium: current concepts, diagnostic dilemmas, and clinical challenges in the post-STICH era. Eur Heart J 2013;34:1323-36.
Schinkel AF, Bax JJ, Poldermans D, et al. Hibernating myocardium: diagnosis and patient outcome. Curr Probl Cardiol 2007;32:375-410.
Pasquet A, Robert A, D¨Hondt AM, et al. Prognosis value of myocardial ischemia and viability in patients with chronic left ventricular ischemia dysfunction. Circulation 1999;100:141-8.
Cleland JG, Calvert M, Freemantle N, et al. Heart failure revascularization trial (HEART). Eur J Heart Fail 2011;13:227-33.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation 2003;107:2900-7.
Allman KC, Shaw LJ, Hachamovitch R, Udelson JE. Myocardial viability testing and impact of revascularization on prognosis in patients with coronary artery disease and left ventricular dysfunction: a meta-analysis. J Am Coll Cardiol 2002;39:1151-8.
Gerber BL, Rousseau MF, Ahn SA, et al. Prognostic value of myocardial viability by delayed-enhanced magnetic resonance in patients with coronary artery disease and low ejection fraction. J Am Coll Cardiol 2012;59: 825-35.
Alderman EL, Fisher LD, Litwin P, et al. Results of coronary artery surgery in patients with por left ventricular function (CASS). Circulation 1983;68:785-95.
Alderman EL, Bourassa MG, Cohen LS, et al. Ten-year follw-up of survival and myocardial infarction in the randomized Coronary Artery Surgery Study. Circulation 1990;82;1629-46.
Velazquez EJ, Lee KL, Jones RH, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Eng J Med 2016;374:1511-20.
Beanlands RS, Nichol G, Huszti E, et al. F-18-fluorodeoxyglucose positron emission tomography imaging-assisted management of patients with severe left ventricular dysfunction and suspected coronary disease: a randomized controlled trial (PARR-2). J Am Coll Cardiol 2007;50:2002-12.
Velazquez EJ, Lee KL, Deja MA, et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Eng J Med 2011;364:1607-16.
Bonow RO, Maurer G, Lee KL, et al. Myocardial viability and survival in ischemic left ventricular dysfunction. N Engl J Med 2011;364:1617-25.
Panza JA, Ellis AM, Al-Khalidi HR. Myocardial viability and long-term outcomes in ischemic cardiomyopathy. N Eng J Med 2019;381:739-48.
Panza JA, Holly TA, Asch FM, et al. Inducible myocardial ischemia and outcomes in patients with coronary artery disease and left ventricular dysfunction. J Am Coll Cardiol 2013;61:1860-70.
Oh JK, Pellikka PA, Panza JA, et al. Core lab analysis of baseline echocardiographic studies in the STICH trial and recommendation for use of echocardiography in future clinical trials. J Am Soc Echocardiogr 2012;25: 327-36.
Schinkel AF, Poldermans D, Rizzello V, et al. Why do patients with ischemic cardiomyopathy and a substantial amount of viable myocardium not always recover in function after revascularization? J Thorac Cardiovasc Surg 2004;127:385-90.
Yusuf S, Zucker D, Peduzzi P, et al. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet 1994;344:563-70.
Cleland JG, Pennell DJ, Ray SG, et al. Myocardial viability as a determinant of the ejection fraction response to carvedilol in patients with heart failure (CHRISTMAS trial). Randomised controlled trial. Lancet 2003;362:14-21.
Samady H, Elefteriades JA, Abbott BG, et al. Failure to improve left ventricular function after coronary revascularization for ischemic cardiomyopathy is not associates with worse outcome. Circulation 1999;100:1298-304.
O’Meara E, Mielniczuk LM, Wells GA, et al., IMAGE HF Investigators. Alternative Imaging Modalities in Ischemic Heart Failure (AIMI-HF) IMAGE HF Project I-A: study protocol for a randomized controlled trial. Trials 2013;14:218.