Acute and long-term success of ventricular tachycardia ablation in patients with ischemic heart disease in a Mexican center
DOI:
https://doi.org/10.47487/apcyccv.v3i4.236Palabras clave:
Ventricular Tachycardia, Ischemic Heart Disease, Catheter AblationResumen
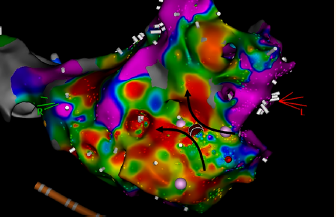
Objective. To report the results of ventricular tachycardia (VT) catheter ablation in ischemic heart disease (IHD), and to identify risk factors associated with recurrence in a Mexican center. Materials and methods. We made a retrospective review of the cases of VT ablation performed in our center from 2015 to 2022. We analyzed the characteristics of the patients and those of the procedures separately and we determined factors associated with recurrence. Results. Fifty procedures were performed in 38 patients (84% male; mean age 58.1 years). Acute success rate was 82%, with a 28% of recurrences. Female sex (OR 3.33, IC 95% 1.66–6.68, p=0.006), atrial fibrillation (OR 3.5, IC 95% 2.08–5.9, p=0.012), electrical storm (OR 2.4, IC 95% 1.06–5.41, p=0.045), functional class greater than II (OR 2.86, IC 95% 1.34–6.10, p=0.018) were risk factors for recurrence and the presence of clinical VT at the time of ablation (OR0.29, IC95% 0.12–0.70, p=0.004) and the use of more than 2 techniques for mapping (OR 0.64, IC 95% 0.48–0.86, p=0.013) were protective factors. Conclusions. Ablation of ventricular tachycardia in ischemic heart disease has had good results in our center. The recurrence is similar to that reported by other authors and there are some factors associated with it.Descargas
Referencias
Dukkipati SR, Koruth JS, Choudry S, Miller MA, Whang W, Reddy VY. Catheter Ablation of Ventricular Tachycardia in Structural Heart Disease: Indications, Strategies, and Outcomes-Part II. J Am Coll Cardiol. 2017;70(23):2924-2941. doi: 10.1016/j.jacc.2017.10.030.
Cronin EM, Bogun FM, Maury P, Peichl P, Chen M, Namboodiri N, et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Europace. 2019;21(8):1143-1144. doi: 10.1093/europace/euz132.
Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter Unsustained Tachycardia Trial Investigators. N Engl J Med. 1999;341(25):1882-90. doi: 10.1056/ NEJM199912163412503.
Reddy VY, Reynolds MR, Neuzil P, Richardson AW, Taborsky M, Jongnarangsin K, et al. Prophylactic catheter ablation for the prevention of defibrillator therapy. N Engl J Med. 2007;357(26):2657- 65. doi: 10.1056/NEJMoa065457
Kuck KH, Schaumann A, Eckardt L, Willems S, Ventura R, Delacrétaz E, et al. Catheter ablation of stable ventricular tachycardia before defibrillator implantation in patients with coronary heart disease (VTACH): a multicentre randomised controlled trial. Lancet. 2010;375(9708):31-40. doi: 10.1016/S0140-6736(09)61755-4.
Sapp JL, Wells GA, Parkash R, Stevenson WG, Blier L, Sarrazin JF, et al. Ventricular Tachycardia Ablation versus Escalation of Antiarrhythmic Drugs. N Engl J Med. 2016;375(2):111-21. doi: 10.1056/NEJMoa1513614.
Kuck KH, Tilz RR, Deneke T, Hoffmann BA, Ventura R, Hansen PS, et al. Impact of Substrate Modification by Catheter Ablation on Implantable Cardioverter-Defibrillator Interventions in Patients With Unstable Ventricular Arrhythmias and Coronary Artery Disease: Results From the Multicenter Randomized Controlled SMS (Substrate Modification Study). Circ Arrhythm Electrophysiol. 2017;10(3):e004422. doi: 10.1161/CIRCEP.116.004422.
Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Executive summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2018;15(10):e190-e252. doi: 10.1016/j.hrthm.2017.10.035.
Vergara P, Roque C, Oloriz T, Mazzone P, Della Bella P. Substrate mapping strategies for successful ablation of ventricular tachycardia: a review. Arch Cardiol Mex. 2013;83(2):104-11. doi: 10.1016/j.acmx.2013.02.001.
Kim YH, Chen SA, Ernst S, Guzman CE, Han S, Kalarus Z, et al. 2019 APHRS expert consensus statement on three-dimensional mapping systems for tachycardia developed in collaboration with HRS, EHRA, and LAHRS. J Arrhythm. 2020;36(2):215-270. doi: 10.1002/joa3.12308.
Sosa E, Scanavacca M, d’Avila A, Pilleggi F. A new technique to perform epicardial mapping in the electrophysiology laboratory. J Cardiovasc Electrophysiol. 1996;7(6):531-6. doi: 10.1111/j.1540- 8167.1996.tb00559.x.
DiBiaseL,SantangeliP,BurkhardtDJ,BaiR,MohantyP,Carbucicchio C, et al. Endo-epicardial homogenization of the scar versus limited substrate ablation for the treatment of electrical storms in patients with ischemic cardiomyopathy. J Am Coll Cardiol. 2012;60(2):132-41. doi: 10.1016/j.jacc.2012.03.044.
Nakahara S, Tung R, Ramirez RJ, Michowitz Y, Vaseghi M, Buch E, et al. Characterization of the arrhythmogenic substrate in ischemic and nonischemic cardiomyopathy implications for catheter ablation of hemodynamically unstable ventricular tachycardia. J Am Coll Cardiol. 2010;55(21):2355-65. doi: 10.1016/j.jacc.2010.01.041.
Di Biase L, Burkhardt JD, Lakkireddy D, Carbucicchio C, Mohanty S, Mohanty P, et al. Ablation of Stable VTs Versus Substrate Ablation in Ischemic Cardiomyopathy: The VISTA Randomized Multicenter Trial. J Am Coll Cardiol. 2015;66(25):2872-2882. doi: 10.1016/j. jacc.2015.10.026.
Wolf M, Sacher F, Cochet H, Kitamura T, Takigawa M, Yamashita S, et al. Long-Term Outcome of Substrate Modification in Ablation of Post-Myocardial Infarction Ventricular Tachycardia. Circ Arrhythm Electrophysiol. 2018;11(2):e005635. doi: 10.1161/CIRCEP.117.005635.
Briceño DF, Romero J, Villablanca PA, Londoño A, Diaz JC, Maraj I, et al. Long-term outcomes of different ablation strategies for ventricular tachycardia in patients with structural heart disease: systematic review and meta-analysis. Europace. 2018;1;20(1):104-115. doi: 10.1093/europace/eux109.
Tung R, Michowitz Y, Yu R, Mathuria N, Vaseghi M, Buch E, et al. Epicardial ablation of ventricular tachycardia: an institutional experience of safety and efficacy. Heart Rhythm. 2013;10(4):490-8. doi: 10.1016/j.hrthm.2012.12.013.
Vergara P, Trevisi N, Ricco A, Petracca F, Baratto F, Cireddu M, et al. Late potentials abolition as an additional technique for reduction of arrhythmia recurrence in scar related ventricular tachycardia ablation. J Cardiovasc Electrophysiol. 2012;23(6):621-7. doi: 10.1111/j.1540-8167.2011.02246.x.
Siontis KC, Kim HM, Stevenson WG, Fujii A, Bella PD, Vergara P, et al. Prognostic Impact of the Timing of Recurrence of Infarct-Related Ventricular Tachycardia After Catheter Ablation. Circ Arrhythm Electrophysiol. 2016;9(12):e004432. doi: 10.1161/CIRCEP.116.004432.
Lam CSP, Arnott C, Beale AL, Chandramouli C, Hilfiker-Kleiner D, Kaye DM, et al. Sex differences in heart failure. Eur Heart J. 2019;40(47):3859-3868c. doi: 10.1093/eurheartj/ehz835.
Ehdaie A, Cingolani E, Shehata M, Wang X, Curtis AB, Chugh SS. Sex Differences in Cardiac Arrhythmias: Clinical and Research Implications. Circ Arrhythm Electrophysiol. 2018;11(3):e005680. doi: 10.1161/CIRCEP.117.005680.
Haanschoten DM, Smit JJJ, Adiyaman A, Ramdat Misier AR, Hm Delnoy PP, Elvan A. Long-term outcome of catheter ablation in post-infarction recurrent ventricular tachycardia. Scand Cardiovasc J. 2019;53(2):62-70. doi: 10.1080/14017431.2019.1601253.
Vergara P, Tzou WS, Tung R, Brombin C, Nonis A, Vaseghi M, et al. Predictive Score for Identifying Survival and Recurrence Risk Profiles in Patients Undergoing Ventricular Tachycardia Ablation: The I-VT Score. Circ Arrhythm Electrophysiol. 2018;11(12):e006730. doi: 10.1161/CIRCEP.118.006730.
Acosta J, Fernández-Armenta J, Penela D, Andreu D, Borras R, Vassanelli F, et al. Infarct transmurality as a criterion for first-line endo-epicardial substrate-guided ventricular tachycardia ablation in ischemic cardiomyopathy. Heart Rhythm. 2016;13(1):85-95. doi: 10.1016/j.hrthm.2015.07.010.
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2022 La revista es titular de la primera publicación, luego el autor dando crédito a la primera publicación.

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.


















